Julie R. Gralow, MD Director, Breast Medical Oncology, Seattle
реклама
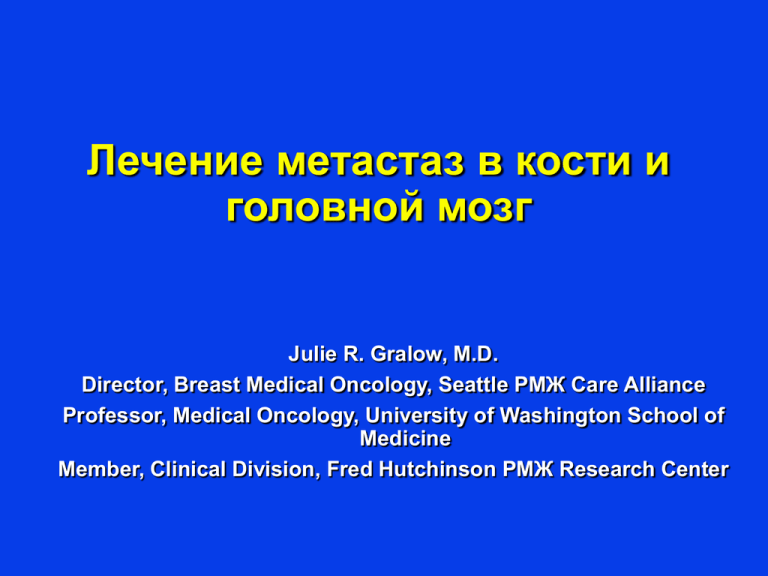
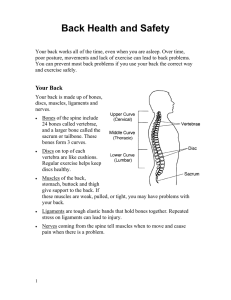
Лечение метастаз в кости и головной мозг Julie R. Gralow, M.D. Director, Breast Medical Oncology, Seattle РМЖ Care Alliance Professor, Medical Oncology, University of Washington School of Medicine Member, Clinical Division, Fred Hutchinson РМЖ Research Center Рецидивы при метастатическом РМЖ Первичная область рецидива Более поздний рецидив • Кости 35-45% 65-70% • Легкие 15-25% 35-45% (плевральныйPleural effusions) • Печень 5-10% 30-40% • ЦНС редко 10-15% Аутопсия series 49-74% 55-77% (50%) 50-75% 20-40% • В общем, рецидив РМЖ является системным и появляется во многих органах Костные метастазы при РМЖ • 65-75% пациентов с метастатическим РМЖ имеют нарушения в костях • 50-70% пациентов с метастатическим поражением костей experience SREs Средняя выживаемость: • ~ 2 года, при 20% 5летн. выживаемости (Coleman 1997) • ~ 4 года (Giordano 2004, Van Poznak 2005) Осложнения при РМЖ с метастазами в костную ткань • • • • • Боль Патологические переломы Компрессия спинного мозга Гиперкальциемия Лечение Skeletal осложнений составляют 63% больничных расходов, связанных с ведением больных с advanced РМЖ (Coleman, РМЖ 80:1588-1594, 1997) Лечение РМЖ с метастазами в костную ткань • • • • • Обезболивание Системная противораковая терапия Ортопедические вмешательства Лучевая терапия и радиоизотопы Ингибиторы остеокластов Osteoclast inhibition Показания для ортопедических вмешательств • Коррекция патологических переломов • Профилактика impending переломов – Большинство больных без переломов не нуждаются в хирургических вмешательствах • лечение/профилактика компрессий спинного мозга Scoring Система предсказания возникновения патологических переломов, обусловленных метастазами в костную ткань Mirels H et al, Clin Ortho 2003 Variable Область Боль Радиограф Размер (% of shaft) Score 0-6 7 8 9 10 Points 1 2 3 верхн. ext ниж. ext peri-trochanteric mild moderate mechanical blastic смешан. lytic 0-33 пациенты (n) 11 19 12 7 18 34-67 68-100 частота переломов 0% 5% Recommend surgery 33% for score > 8 57% 100% Наружная Beam лучевая терапия • Показания – Освобождение от боли и профилактика переломовs • Польза – Обезболивание, как минимум частично у 80-90% пациентов – Костные метастазы с наиболее выраженными симптомами начинают реагировать через 10-14 дней – Долгосрочный обезболивающий эффект (> 6-12 месяцев) • Лимитация – Местное применение – Многочисленные курсы радиотерапии – Кумулятивный супрессивный эффект на костный мозг • Дебаты в области оптимальных доз и продолжительности лечения кости-seeking Radionuclides Mertens WC et al, CA РМЖ J Clin 48:361-374, 1998 • FDA approved: 32P, 89Strontium, 153Samarium-EDTMP • Greater experience in prostate than in breast due to lack of other systemic лечениеs and less visceral involvement • Strengths – Systemic, addresses all sites of кости involvement – Selective absorption into кости, delivers energy locally with minimal systemic effects – Single IV dose produces pain relief in the majority of пациенты • Limitations – Effect shorter-lived than external beam; reлечение or other therapy required – Transient marrow suppression limits concurrent use with chemotherapy – Acute leukemia risk with 32P Osteoclast Inhibition • • • • Bisphosphonates RANK ligand inhibitors Gallium nitrate Under investigation: – Cathepsin K inhibitors – Src kinase inhibitors Breast РМЖ and Osteoclast Inhibition PTHrP, prostaglandins, interleukins, RANK-L osteoblasts, macrophages breast РМЖ cells osteoclasts IGF, PDGF, TGF-B Bisphosphonates in Treating кости метастазы in Breast РМЖ • Several bisphosphonates approved throughout the world for reduction in skeletalrelated complications in пациенты with кости метастазы – clodronate (po) – pamidronate (IV) - US – zoledronic acid (IV) - US – ibandronate (IV, po) • To date, no improvement in выживаемость has been seen in метастатический breast РМЖ In Vitro Potency of Bisphosphonates Non-nitrogen containing etidronate (Didronel) clodronate (костиfos) Nitrogen containing pamidronate (Aredia) alendronate (Fosamax) risedronate (Actonel) ibandronate (Bondronat) zoledronic acid (Zometa) 1 10 100 1,000 5,000-10,000 10,000 20,000 Bisphosphonates Reduce Skeletal Related Events (SRE) in Breast РМЖ % pts with SRE Placebo 65% 24 months 1 Pamidronate 46% Pamidronate 49% 24 months 2 Zoledronic Acid 46% Placebo 50% 12 months 3 Zoledronic Acid 30% (p = not sig) A et al, РМЖ, 2000; 2 Rosen LS et al, РМЖ, 2003; 3 Kohno N et al, J Clin Oncol 23, 2005 1 Lipton Zoledronic Acid vs. Placebo in Stage IV Breast РМЖ Pain Scores (Brief Pain Inventory) Kohno N et al, J Clin Oncol 23, 2005 First -line Denosumab for кости метастазы Denosumab vs. Zoledronic Acid for профилактика of Skeletal-Related Events in Breast РМЖ Stopeck et al, J Clin Oncol 28, 2010 пациенты with кости метастазы due to breast РМЖ R A N D O M I Z E Denosumab 120 mg s.c. Placebo I.V. q 4 weeks (n = 1026) Zoledronic acid 4 mg I.V. Placebo s.c. q 4 weeks (n = 1020) Denosumab is a monoclonal antibody that inhibits osteoclasts through the RANK ligand pathway. It was FDA approved in 2010 Denosumab vs. Zoledronic Acid for профилактика of Skeletal-Related Events in Breast РМЖ Stopeck et al, J Clin Oncol 28, 2010 Denosumab compared to zoledronic acid: • Subcutaneous vs intravenous • Efficacy • 23% reduction for time to first + subsequent SRE (P = .001) • 26% reduction for time to first radiation to кости (P = .01) • 13% reduction for time to moderate/severe pain (P = .009) • Similar overall disease progression • Toxicity • ONJ 20 (denosumab) vs 14 (zoledronic acid) • No renal issues with denosumab – no need for pre-creatinine • Reduced first infusion myalgias/arthralgias with denosumab Breast РМЖ Brain метастазы Brain метастазы in Breast РМЖ • Incidence of CNS метастазы in advanced breast РМЖ – Clinically apparent 10-15% – Autopsy series » Parenchymal 30%, leptomeningeal 5-16% – Higher in HER2+, trastuzumab treated pts? • Factors associated with a longer life expectancy include either well-controlled or no метастазы outside the brain, and being able to carry out daily routines without help лечениеs for Brain метастазы • лечение options for CNS метастазы – Surgical resection – Radiation therapy » Whole brain » Focal radiation (stereotactic, gamma knife) » ?Radiation sensitizers – Systemic therapy – Supportive meds » Corticosteroids, anticonvulsants, pain control Brain Surgery • Used for 1-2 large метастазы (sometimes up to 4), or when метастазы are too big for radiosurgery • Surgery also sometimes done to confirm the diagnosis of brain metastasis – 10% of the time the suspected brain metastasis is something else, like a primary brain tumor, a nonРМЖous mass, or an infection • Whole brain radiation often given after surgery to prevent brain метастазы from recurring – Definitive evidence that WBRT extends life when there is a single brain metastasis • Radiosurgery after surgery can also be used as a “boost” to prevent recurrence at the site of surgery Whole Brain Radiation Therapy (WBRT) • Used for the лечение of multiple brain метастазы, delivered to the entire brain. • Shown to extend life and improvequality of life • 30-40% of пациенты achieve complete reversal of symptoms; 75-85% of пациенты experience some improvement or stabilization of symptoms, especially headache and seizure • Short term side effects include memory loss, particularly verbal memory, fatigue, temporary baldness, skin rash • Factors associated with a longer life expectancy include either well-controlled or no метастазы outside the brain, and being able to carry out daily routines without help • 50% of those who receive WBRT have recurrences in the Stereotactic Radiosurgery (Gammaknife, Cyberknife, X-Knife or Stereotactic Radiosurgery) • Aims high doses of radiation in a targeted manner, minimizing toxicities • Generally not used for more than 3 метастазы at a time, or метастазы larger than 3 centimeters • Severe side effects occur in 1-2%, including seizures, edema, hemorrhage, and radionecrosis • Can be repeated if new brain метастазы appear • Although no direct evidence exists, radiosurgery is thought to be as effective, and safer, than regular surgery for метастазы up to 3 centimeters • Can also be used after regular surgery or WBRT as a “boost” to prevent brain метастазы from recurring • Controversial: whether WBRT is necessary after radiosurgery Systemic Therapies in Treating Brain метастазы • Chemotherapy • Not extensively studied for brain метастазы in breast РМЖ • Most chemo drugs not able to cross the blood-brain barrier • Evidence is emerging that as brain метастазы grow they disrupt the blood-brain barrier, making it possible for chemotherapeutic drugs to get into the brain • Brain метастазы usually occur late in the course of breast РМЖ when resistance to chemo is more likely • Drugs with activity: capecitabine, high-dose mexthotrexate, carboplatin,cisplatin, doxorubicin Systemic Therapies in Treating Brain метастазы • Endocrine Therapy • Tamoxifen, aromatase inhibitors, and megestrol acetate effective in treating ER-positive breast РМЖ brain метастазы • Majority of women with brain метастазы have tumors that are estrogen receptor-negative or endocrineresistant • Hormone status of a brain metastasis can be different from the hormonal status of the primary tumor – Preliminary evidence that in метастазы, including brain метастазы, estrogen receptor, progesterone receptor, and HER2 can hange from positive to negative Lapatinib as 1st-Line лечение in HER-2+ Advanced Breast РМЖ Gomez HL et al, ASCO 2005, abstract #3046 Lapatinib crosses the blood-brain barrier Patient D: Brain Lesion Baseline and 12 Weeks Leptomeningeal метастазы (Carcinomatous Meningitis) • 2-5% of метастатический breast РМЖ пациенты develop leptomeningeal метастазы – Usually occurs at a very late stage • Difficult to treat, since many drugs unable to penetrate into the CSF • Often brain метастазы and leptomeningeal метастазы occur at the same time • No agreed-upon standard лечение – Much of the time, benefits of лечение are offset by лечение side effects Leptomeningeal метастазы (Carcinomatous Meningitis) • лечение depends on whether leptomeningeal метастазы are bulky or small and diffuse • Radiation given to relieve symptoms in areas of bulky disease • Chemotherapy given for diffuse disease; may extend life for several months • No direct evidence that intrathecal chemotherapy is better than intravenous • Intrathecal therapy generally reserved for пациенты whose systemic disease is under control – Methotrexate and cytarabine commonly used – Important to continue to treat other метастатический disease – Usually delivered through an Ommaya reservoir Ommaya Reservoir лечение of метастатический Breast РМЖ: A Balancing Act Balancing лечение efficacy and toxicity is the major objective Quantity of Life Quality of Life