Лечение метастазов печени колоректальной этиологии (с
реклама
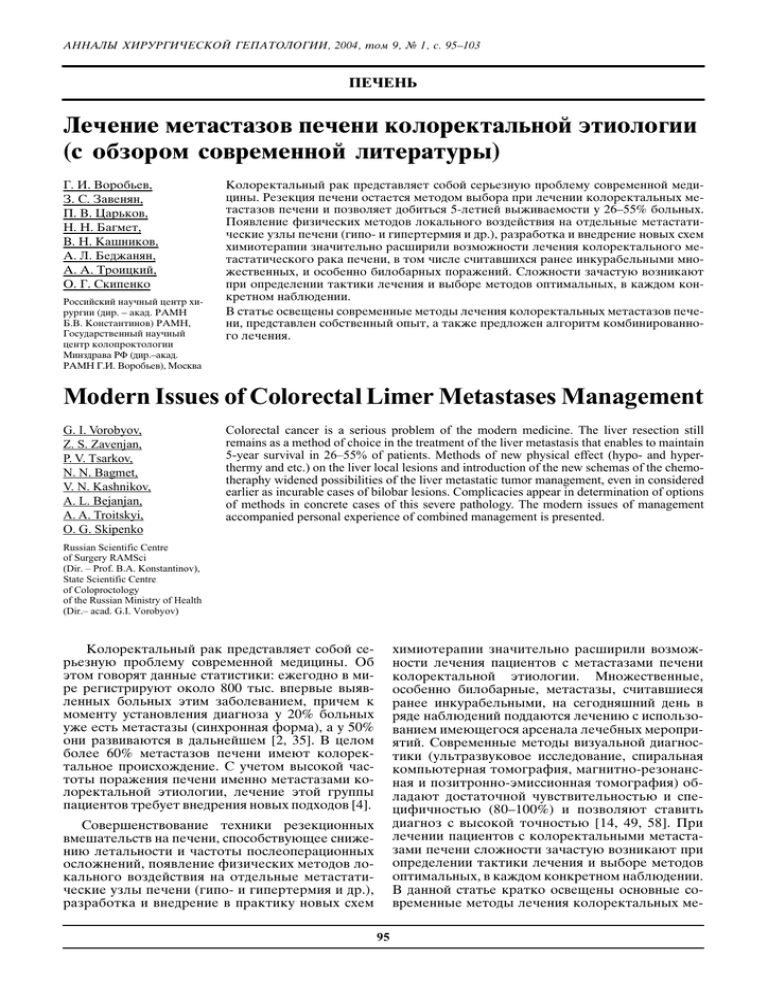
ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà, 2004, ÚÓÏ 9, ‹ 1, Ò. 95–103 Ô˜Â̸ ã˜ÂÌË ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË (Ò Ó·ÁÓÓÏ ÒÓ‚ÂÏÂÌÌÓÈ ÎËÚ‡ÚÛ˚) É. à. ÇÓÓ·¸Â‚, á. ë. ᇂÂÌflÌ, è. Ç. ñ‡¸ÍÓ‚, ç. ç. Ň„ÏÂÚ, Ç. ç. 䇯ÌËÍÓ‚, Ä. ã. ʼnʇÌflÌ, Ä. Ä. íÓˈÍËÈ, é. É. ëÍËÔÂÌÍÓ êÓÒÒËÈÒÍËÈ Ì‡Û˜Ì˚È ˆÂÌÚ ıËÛ„ËË (‰Ë. – ‡Í‡‰. êÄåç Å.Ç. äÓÌÒÚ‡ÌÚËÌÓ‚) êÄåç, ÉÓÒÛ‰‡ÒÚ‚ÂÌÌ˚È Ì‡Û˜Ì˚È ˆÂÌÚ ÍÓÎÓÔÓÍÚÓÎÓ„ËË åËÌÁ‰‡‚‡ êî (‰Ë.–‡Í‡‰. êÄåç É.à. ÇÓÓ·¸Â‚), åÓÒÍ‚‡ äÓÎÓÂÍڇθÌ˚È ‡Í Ô‰ÒÚ‡‚ÎflÂÚ ÒÓ·ÓÈ Ò¸ÂÁÌÛ˛ ÔÓ·ÎÂÏÛ ÒÓ‚ÂÏÂÌÌÓÈ Ï‰ˈËÌ˚. êÂÁÂ͈Ëfl Ô˜ÂÌË ÓÒÚ‡ÂÚÒfl ÏÂÚÓ‰ÓÏ ‚˚·Ó‡ ÔË Î˜ÂÌËË ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË Ë ÔÓÁ‚ÓÎflÂÚ ‰Ó·ËÚ¸Òfl 5-ÎÂÚÌÂÈ ‚˚ÊË‚‡ÂÏÓÒÚË Û 26–55% ·ÓθÌ˚ı. èÓfl‚ÎÂÌË ÙËÁ˘ÂÒÍËı ÏÂÚÓ‰Ó‚ ÎÓ͇θÌÓ„Ó ‚ÓÁ‰ÂÈÒÚ‚Ëfl ̇ ÓÚ‰ÂθÌ˚ ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍË ÛÁÎ˚ Ô˜ÂÌË („ËÔÓ- Ë „ËÔÂÚÂÏËfl Ë ‰.), ‡Á‡·ÓÚ͇ Ë ‚̉ÂÌË ÌÓ‚˚ı ÒıÂÏ ıËÏËÓÚ‡ÔËË Á̇˜ËÚÂθÌÓ ‡Ò¯ËËÎË ‚ÓÁÏÓÊÌÓÒÚË Î˜ÂÌËfl ÍÓÎÓÂÍڇθÌÓ„Ó ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍÓ„Ó ‡Í‡ Ô˜ÂÌË, ‚ ÚÓÏ ˜ËÒΠҘËÚ‡‚¯ËıÒfl ‡Ì ËÌÍÛ‡·ÂθÌ˚ÏË ÏÌÓÊÂÒÚ‚ÂÌÌ˚ı, Ë ÓÒÓ·ÂÌÌÓ ·ËÎÓ·‡Ì˚ı ÔÓ‡ÊÂÌËÈ. ëÎÓÊÌÓÒÚË Á‡˜‡ÒÚÛ˛ ‚ÓÁÌË͇˛Ú ÔË ÓÔ‰ÂÎÂÌËË Ú‡ÍÚËÍË Î˜ÂÌËfl Ë ‚˚·Ó ÏÂÚÓ‰Ó‚ ÓÔÚËχθÌ˚ı, ‚ ͇ʉÓÏ ÍÓÌÍÂÚÌÓÏ Ì‡·Î˛‰ÂÌËË. Ç Òڇڸ ÓÒ‚Â˘ÂÌ˚ ÒÓ‚ÂÏÂÌÌ˚ ÏÂÚÓ‰˚ ΘÂÌËfl ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË, Ô‰ÒÚ‡‚ÎÂÌ ÒÓ·ÒÚ‚ÂÌÌ˚È ÓÔ˚Ú, ‡ Ú‡ÍÊ Ô‰ÎÓÊÂÌ ‡Î„ÓËÚÏ ÍÓÏ·ËÌËÓ‚‡ÌÌÓ„Ó Î˜ÂÌËfl. Modern Issues of Colorectal Limer Metastases Management G. I. Vorobyov, Z. S. Zavenjan, P. V. Tsarkov, N. N. Bagmet, V. N. Kashnikov, A. L. Bejanjan, A. A. Troitskyi, O. G. Skipenko Colorectal cancer is a serious problem of the modern medicine. The liver resection still remains as a method of choice in the treatment of the liver metastasis that enables to maintain 5-year survival in 26–55% of patients. Methods of new physical effect (hypo- and hyperthermy and etc.) on the liver local lesions and introduction of the new schemas of the chemotheraphy widened possibilities of the liver metastatic tumor management, even in considered earlier as incurable cases of bilobar lesions. Complicacies appear in determination of options of methods in concrete cases of this severe pathology. The modern issues of management accompanied personal experience of combined management is presented. Russian Scientific Centre of Surgery RAMSci (Dir. – Prof. B.A. Konstantinov), State Scientific Centre of Coloproctology of the Russian Ministry of Health (Dir.– acad. G.I. Vorobyov) äÓÎÓÂÍڇθÌ˚È ‡Í Ô‰ÒÚ‡‚ÎflÂÚ ÒÓ·ÓÈ Ò¸ÂÁÌÛ˛ ÔÓ·ÎÂÏÛ ÒÓ‚ÂÏÂÌÌÓÈ Ï‰ˈËÌ˚. é· ˝ÚÓÏ „Ó‚ÓflÚ ‰‡ÌÌ˚ ÒÚ‡ÚËÒÚËÍË: ÂÊ„ӉÌÓ ‚ ÏË „ËÒÚËÛ˛Ú ÓÍÓÎÓ 800 Ú˚Ò. ‚Ô‚˚ ‚˚fl‚ÎÂÌÌ˚ı ·ÓθÌ˚ı ˝ÚËÏ Á‡·Ó΂‡ÌËÂÏ, Ô˘ÂÏ Í ÏÓÏÂÌÚÛ ÛÒÚ‡ÌÓ‚ÎÂÌËfl ‰Ë‡„ÌÓÁ‡ Û 20% ·ÓθÌ˚ı ÛÊ ÂÒÚ¸ ÏÂÚ‡ÒÚ‡Á˚ (ÒËÌıÓÌ̇fl ÙÓχ), ‡ Û 50% ÓÌË ‡Á‚Ë‚‡˛ÚÒfl ‚ ‰‡Î¸ÌÂȯÂÏ [2, 35]. Ç ˆÂÎÓÏ ·ÓΠ60% ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË ËÏÂ˛Ú ÍÓÎÓÂÍڇθÌÓ ÔÓËÒıÓʉÂÌËÂ. ë Û˜ÂÚÓÏ ‚˚ÒÓÍÓÈ ˜‡ÒÚÓÚ˚ ÔÓ‡ÊÂÌËfl Ô˜ÂÌË ËÏÂÌÌÓ ÏÂÚ‡ÒÚ‡Á‡ÏË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË, ΘÂÌË ˝ÚÓÈ „ÛÔÔ˚ Ô‡ˆËÂÌÚÓ‚ Ú·ÛÂÚ ‚̉ÂÌËfl ÌÓ‚˚ı ÔÓ‰ıÓ‰Ó‚ [4]. ıËÏËÓÚ‡ÔËË Á̇˜ËÚÂθÌÓ ‡Ò¯ËËÎË ‚ÓÁÏÓÊÌÓÒÚË Î˜ÂÌËfl Ô‡ˆËÂÌÚÓ‚ Ò ÏÂÚ‡ÒÚ‡Á‡ÏË Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË. åÌÓÊÂÒÚ‚ÂÌÌ˚Â, ÓÒÓ·ÂÌÌÓ ·ËÎÓ·‡Ì˚Â, ÏÂÚ‡ÒÚ‡Á˚, Ò˜ËÚ‡‚¯ËÂÒfl ‡Ì ËÌÍÛ‡·ÂθÌ˚ÏË, ̇ Ò„ӉÌfl¯ÌËÈ ‰Â̸ ‚ fl‰Â ̇·Î˛‰ÂÌËÈ ÔÓ‰‰‡˛ÚÒfl ΘÂÌ˲ Ò ËÒÔÓθÁÓ‚‡ÌËÂÏ Ëϲ˘Â„ÓÒfl ‡ÒÂ̇· Θ·Ì˚ı ÏÂÓÔËflÚËÈ. ëÓ‚ÂÏÂÌÌ˚ ÏÂÚÓ‰˚ ‚ËÁۇθÌÓÈ ‰Ë‡„ÌÓÒÚËÍË (ÛθڇÁ‚ÛÍÓ‚Ó ËÒÒΉӂ‡ÌËÂ, ÒÔˇθ̇fl ÍÓÏÔ¸˛ÚÂ̇fl ÚÓÏÓ„‡ÙËfl, χ„ÌËÚÌÓ-ÂÁÓ̇ÌÒ̇fl Ë ÔÓÁËÚÓÌÌÓ-˝ÏËÒÒËÓÌ̇fl ÚÓÏÓ„‡ÙËfl) ӷ·‰‡˛Ú ‰ÓÒÚ‡ÚÓ˜ÌÓÈ ˜Û‚ÒÚ‚ËÚÂθÌÓÒÚ¸˛ Ë ÒÔˆËÙ˘ÌÓÒÚ¸˛ (80–100%) Ë ÔÓÁ‚ÓÎfl˛Ú ÒÚ‡‚ËÚ¸ ‰Ë‡„ÌÓÁ Ò ‚˚ÒÓÍÓÈ ÚÓ˜ÌÓÒÚ¸˛ [14, 49, 58]. èË Î˜ÂÌËË Ô‡ˆËÂÌÚÓ‚ Ò ÍÓÎÓÂÍڇθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË Ô˜ÂÌË ÒÎÓÊÌÓÒÚË Á‡˜‡ÒÚÛ˛ ‚ÓÁÌË͇˛Ú ÔË ÓÔ‰ÂÎÂÌËË Ú‡ÍÚËÍË Î˜ÂÌËfl Ë ‚˚·Ó ÏÂÚÓ‰Ó‚ ÓÔÚËχθÌ˚ı, ‚ ͇ʉÓÏ ÍÓÌÍÂÚÌÓÏ Ì‡·Î˛‰ÂÌËË. Ç ‰‡ÌÌÓÈ Òڇڸ ͇ÚÍÓ ÓÒ‚Â˘ÂÌ˚ ÓÒÌÓ‚Ì˚ ÒÓ‚ÂÏÂÌÌ˚ ÏÂÚÓ‰˚ ΘÂÌËfl ÍÓÎÓÂÍڇθÌ˚ı ÏÂ- ëӂ¯ÂÌÒÚ‚Ó‚‡ÌË ÚÂıÌËÍË ÂÁÂ͈ËÓÌÌ˚ı ‚ϯ‡ÚÂθÒÚ‚ ̇ Ô˜ÂÌË, ÒÔÓÒÓ·ÒÚ‚Û˛˘Â ÒÌËÊÂÌ˲ ÎÂڇθÌÓÒÚË Ë ˜‡ÒÚÓÚ˚ ÔÓÒÎÂÓÔ‡ˆËÓÌÌ˚ı ÓÒÎÓÊÌÂÌËÈ, ÔÓfl‚ÎÂÌË ÙËÁ˘ÂÒÍËı ÏÂÚÓ‰Ó‚ ÎÓ͇θÌÓ„Ó ‚ÓÁ‰ÂÈÒÚ‚Ëfl ̇ ÓÚ‰ÂθÌ˚ ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍË ÛÁÎ˚ Ô˜ÂÌË („ËÔÓ- Ë „ËÔÂÚÂÏËfl Ë ‰.), ‡Á‡·ÓÚ͇ Ë ‚̉ÂÌË ‚ Ô‡ÍÚËÍÛ ÌÓ‚˚ı ÒıÂÏ 95 Ô˜Â̸ ãÖóÖçàÖ åÖíÄëíÄáéÇ èÖóÖçà äéãéêÖäíÄãúçéâ ùíàéãéÉàà 퇷Îˈ‡ 1. éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ÂÁÂ͈ËÈ Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ä‚ÚÓ˚ ÉÓ‰ óËÒÎÓ èflÚËÎÂÚÌflfl ÓÔ‡- ‚˚ÊË‚‡ÂˆËÈ ÏÓÒÚ¸, % 퇷Îˈ‡ 2. èflÚËÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÔÓÒΠÂÁÂ͈ËË Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÏÌÓÊÂÒÚ‚ÂÌÌ˚ı ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ [34] óËÒÎÓ ÏÂÚ‡ÒÚ‡ÁÓ‚ Ç˚ÊË‚‡ÂÏÓÒÚ¸, % 1 37 D. Nadig Ë ÒÓ‡‚Ú. [47] 1997 275 26 K. Hardy Ë ÒÓ‡‚Ú. [27] 1998 100 55 2 34 Y. Fong Ë ÒÓ‡‚Ú. [21] 1999 1001 37 3 9 M. Minagawa Ë ÒÓ‡‚Ú. [44] 2000 235 38 4 18 Ú‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË Ë ÔÛÚË Â¯ÂÌËfl ÌÂÍÓÚÓ˚ı Ú‡ÍÚ˘ÂÒÍËı Á‡‰‡˜. ã˜ÂÌË ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË êÂÁÂ͈Ëfl Ô˜ÂÌË. ç‡ Ò„ӉÌfl¯ÌËÈ ‰Â̸ ÏÂÚÓ‰ÓÏ ‚˚·Ó‡ ÔË Î˜ÂÌËË Ô‡ˆËÂÌÚÓ‚ Ò ÍÓÎÓÂÍڇθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË Ô˜ÂÌË fl‚ÎflÂÚÒfl  ÂÁÂ͈Ëfl [28]. ë‰Ìflfl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË Ô‡ˆËÂÌÚÓ‚ Ò ÍÓÎÓÂÍڇθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË, ÔÓÎÛ˜‡‚¯ËÏË ÚÓθÍÓ ÒËÏÔÚÓχÚ˘ÂÒÍӠΘÂÌËÂ, Ì Ô‚˚¯‡ÂÚ 5 ÏÂÒ [11]. èË ‚˚ÔÓÎÌÂÌËË ÂÁÂ͈ËË Ô˜ÂÌË ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË Ô‡ˆËÂÌÚÓ‚ Û‚Â΢˂‡ÂÚÒfl Ë 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÍÓηÎÂÚÒfl ÓÚ 22 ‰Ó 55 % [56] (Ú‡·Î. 1). ÑÂڇθÌÓ ËÁÛ˜ÂÌË ‡Ì‡ÚÓÏËË Ô˜ÂÌË Ë Òӂ¯ÂÌÒÚ‚Ó‚‡ÌË ÚÂıÌËÍË ÓÔ‡ÚË‚Ì˚ı ‚ϯ‡ÚÂθÒÚ‚ ÔÓÁ‚ÓÎËÎË Á̇˜ËÚÂθÌÓ ÛÏÂ̸¯ËÚ¸ ˜ËÒÎÓ ÔÓÒÎÂÓÔ‡ˆËÓÌÌ˚ı ÓÒÎÓÊÌÂÌËÈ (15–35%) Ë ÎÂڇθÌÓÒÚ¸ (0–11%, Ô˘ÂÏ ‚ ·Óθ¯ËÌÒڂ ωˈËÌÒÍËı ˆÂÌÚÓ‚ Ó̇ ÌËÊ 5%) ÔË ‚˚ÔÓÎÌÂÌËË ÂÁÂ͈ËÈ Ô˜ÂÌË [13, 19, 20, 34]. èÓ ÔÓ‚Ó‰Û ÓÔÚËχθÌ˚ı ÒÓÍÓ‚ ‚˚ÔÓÎÌÂÌËfl ÂÁÂ͈ËË Ô˜ÂÌË ÒÛ˘ÂÒÚ‚ÛÂÚ ÌÂÒÍÓθÍÓ ÏÌÂÌËÈ. ë Ó‰ÌÓÈ ÒÚÓÓÌ˚, ÓÔ‡ˆË˛ ÌÛÊÌÓ ÔÓ‚Ó‰ËÚ¸ Í‡Í ÏÓÊÌÓ ÒÍÓ ÔÓÒΠÛÒÚ‡ÌÓ‚ÎÂÌËfl ‰Ë‡„ÌÓÁ‡ Ò ˆÂθ˛ ÔÓÙË·ÍÚËÍË ‚ÓÁÏÓÊÌÓ„Ó ÎËÏÙÓ- Ë „ÂχÚÓ„ÂÌÌÓ„Ó ‡ÒÔÓÒÚ‡ÌÂÌËfl ÔÓˆÂÒÒ‡. A. Lambert Ë ÒÓ‡‚Ú. Ô‰·„‡˛Ú ‰ËÙÙÂÂ̈ËÓ‚‡ÌÌ˚È ÔÓ‰ıÓ‰ Í Â¯ÂÌ˲ ˝ÚÓÈ ÔÓ·ÎÂÏ˚ [38]. èÓ Ëı ‰‡ÌÌ˚Ï, Ôӂ‰ÂÌË ÍÓÌÚÓθÌÓÈ ÍÓÏÔ¸˛ÚÂÌÓÈ ÚÓÏÓ„‡ÙËË ‚ ÒÓÍË ÓÚ 2 ‰Ó 6 ÏÂÒ ÔÓÒΠ‚˚fl‚ÎÂÌËfl Ô˜ÂÌÓ˜Ì˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ì Ó͇Á˚‚‡ÂÚ Ì··„ÓÔËflÚÌÓ„Ó ‚ÎËflÌËfl ̇ ÔÓ„ÌÓÁ. êÂÁÂÍˆË˛ ‚˚ÔÓÎÌfl˛Ú ÚÓθÍÓ ÚÂÏ Ô‡ˆËÂÌÚ‡Ï, Û ÍÓÚÓ˚ı Ì ‚ÓÁÌË͇˛Ú ÌÓ‚˚ ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍË ÛÁÎ˚. í‡Í Í‡Í Á‡ ‚ÂÏfl ̇·Î˛‰ÂÌËfl ÍÛÔÌ˚ ÏÂÚ‡ÒÚ‡Á˚ ÏÓ„ÛÚ ÒÚ‡Ú¸ ÌÂÂÁÂÍÚ‡·ÂθÌ˚ÏË (̇ÔËÏÂ, ‚ÒΉÒÚ‚Ë ÔÓ‡ÒÚ‡ÌËfl ÓÔÛıÓÎË ‚ ÓÒÌÓ‚Ì˚ ÒÓÒÛ‰ËÒÚ˚ ÒÚÛÍÚÛ˚ ËÎË ‡ÒÔÓÒÚ‡ÌÂÌËfl ̇ ÒÓÒ‰ÌË ӷ·ÒÚË), ÍÛÔÌ˚ ÛÁÎ˚ (·ÓΠ4 ÒÏ) ÌÂÓ·ıÓ‰ËÏÓ ÂÁˆËÓ‚‡Ú¸ ·ÂÁ ÔÓωÎÂÌËfl. ë ‰Û„ÓÈ ÒÚÓÓÌ˚, ÏÂÎÍË ÏÂÚ‡ÒÚ‡Á˚ (ÏÂÌ 1 ÒÏ), ÓÒÓ·ÂÌÌÓ ÂÒÎË ÓÌË ‡ÒÔÓÎÓÊÂÌ˚ ‚ ÌÂÒÍÓθÍËı Ò„ÏÂÌÚ‡ı Ë ÚÂ·Û˛Ú ‚˚ÔÓÎÌÂÌËfl ·Óθ¯ÓÈ ÂÁÂ͈ËË, ÒΉÛÂÚ ÓÔÂËÓ‚‡Ú¸ ˜ÂÂÁ 3 ÏÂÒ ÔÓÒΠÍÓÌÚÓθÌÓÈ ÍÓÏÔ¸˛ÚÂÌÓÈ ÚÓÏÓ„‡ÙËË. èÓ ÏÌÂÌ˲ Ä. Lambert Ë 96 ÒÓ‡‚Ú. ڇ͇fl Ú‡ÍÚË͇ ÔÓÁ‚ÓÎËÚ ‚˚‰ÂÎËÚ¸ Ô‡ˆËÂÌÚÓ‚ ÒÓ ÒÚÂÏËÚÂθÌ˚Ï ÔÓ„ÂÒÒËÓ‚‡ÌËÂÏ Á‡·Ó΂‡ÌËfl, Ëϲ˘Ëı Ì··„ÓÔËflÚÌ˚È ÔÓ„ÌÓÁ. Ç˚ÔÓÎÌÂÌË ÂÁÂ͈ËË Ô˜ÂÌË ‚ÓÁÏÓÊÌÓ Ó‰ÌÓ‚ÂÏÂÌÌÓ Ò Û‰‡ÎÂÌËÂÏ Ô‚˘ÌÓÈ ÓÔÛıÓÎË Í˯ÍË ËÎË ‚ÚÓ˚Ï ˝Ú‡ÔÓÏ, ˜ÚÓ ‚Ó ÏÌÓ„ÓÏ ÓÔ‰ÂÎflÂÚÒfl ÎÓ͇ÎËÁ‡ˆËÂÈ Ô‚˘ÌÓÈ ÓÔÛıÓÎË Ë ÏÂÚ‡ÒÚ‡Á‡. é·˚˜ÌÓ ÒËÌıÓÌÌÓ Û‰‡ÂÚÒfl ‚˚ÔÓÎÌËÚ¸ Ò„ÏÂÌÚ- Ë ·ËÒ„ÏÂÌÚ˝ÍÚÓÏ˲, ‡ Ú‡ÍÊ ‡ÚËÔ˘ÌÛ˛ ÂÁÂÍˆË˛. J. Sheele Ë ÒÓ‡‚Ú. [61] Ì ÂÍÓÏÂÌ‰Û˛Ú ‚˚ÔÓÎÌflÚ¸ ·Óθ¯Ë ‡Ì‡ÚÓÏ˘ÂÒÍË ÂÁÂ͈ËË Ô˜ÂÌË Ó‰ÌÓ‚ÂÏÂÌÌÓ Ò Î˛·˚Ï ‚‡Ë‡ÌÚÓÏ ÂÁÂ͈ËË Í˯ÍË. èË ıËۄ˘ÂÒÍÓÏ Î˜ÂÌËË ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ ıËÛ„Ë ‚Ò ˜‡˘Â ÓÚ͇Á˚‚‡˛ÚÒfl ÓÚ ‚˚ÔÓÎÌÂÌËfl ‡ÚËÔ˘ÌÓÈ ÂÁÂ͈ËË Ô˜ÂÌË, ÓÚ‰‡‚‡fl Ô‰ÔÓ˜ÚÂÌË ‡Ì‡ÚÓÏ˘ÂÒÍÓÈ ÂÁÂ͈ËË („ÂÏË„ÂÔ‡Ú˝ÍÚÓÏËfl, Ò„ÏÂÌÚ˝ÍÚÓÏËfl). àÒÒΉӂ‡ÌË R. DeMatteo Ë ÒÓ‡‚Ú. [17]Ì ‚˚fl‚ËÎÓ ‡Á΢ËÈ ‚ Ó·˙ÂÏ ÍÓ‚ÓÔÓÚÂË, ‚ÂÏÂÌË ÓÔ‡ˆËË, ˜‡ÒÚÓÚÂ Ë ı‡‡ÍÚ ÓÒÎÓÊÌÂÌËÈ ÔË ‚˚ÔÓÎÌÂÌËË ‡ÚËÔ˘ÌÓÈ Ë ‡Ì‡ÚÓÏ˘ÂÒÍÓÈ ÂÁÂ͈ËË. é‰Ì‡ÍÓ ‚ ÒÎÛ˜‡Â ‡Ì‡ÚÓÏ˘ÂÒÍÓÈ ÂÁÂ͈ËË Á̇˜ËÚÂθÌÓ ÒÌËÁË·Ҹ ˜‡ÒÚÓÚ‡ ӷ̇ÛÊÂÌËfl ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ ‚ ͇ Ô˜ÂÌÓ˜ÌÓÈ Ú͇ÌË, ÓÒÚ‡‚¯ÂÈÒfl ÔÓÒΠÂÁÂ͈ËË Ò 16 ‰Ó 2%, ωˇ̇ ÊËÁÌË ‚˚ÓÒ· Ò 38 ‰Ó 53 ÏÂÒ. åÌÓ„Ó˜ËÒÎÂÌÌ˚ÏË ËÒÒΉӂ‡ÌËflÏË ·˚Î ‚˚fl‚ÎÂÌ fl‰ Ù‡ÍÚÓÓ‚, ‚ÎËfl˛˘Ëı ̇ ÔÓ„ÌÓÁ ÔË ÂÁÂ͈ËË Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ ‚ Ô˜Â̸. 1. ê‡ÒÒÚÓflÌË ÓÚ Í‡fl ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍÓ„Ó ÛÁ· ‰Ó ÎËÌËË ÂÁÂ͈ËË. ÑÓ Ò‰ËÌ˚ 90-ı „Ó‰Ó‚ Ò˜ËÚ‡ÎÓÒ¸, ˜ÚÓ ‡ÒÒÚÓflÌË ÓÚ Í‡fl ÏÂÚ‡ÒÚ‡Á‡ ‰Ó ÎËÌËË ÂÁÂ͈ËË Ì ‰ÓÎÊÌÓ ·˚Ú¸ ÏÂÌ 1 ÒÏ [13]. àÒÒΉӂ‡ÌËfl, Ôӂ‰ÂÌÌ˚ Á‡ ÔÓÒΉÌË ÌÂÒÍÓθÍÓ ÎÂÚ Ë Ò‡‚ÌË‚‡‚¯Ë ‰Ó‚ÓθÌÓ ·Óθ¯Ë „ÛÔÔ˚ Ô‡ˆËÂÌÚÓ‚ (·ÓΠ80), Ì ‚˚fl‚ËÎË ‰ÓÒÚÓ‚ÂÌÓÈ ‡ÁÌˈ˚ ‚ ‚˚ÊË‚‡ÂÏÓÒÚË ÒÂ‰Ë Ô‡ˆËÂÌÚÓ‚, Û ÍÓÚÓ˚ı ‡ÒÒÚÓflÌË ‰Ó ÎËÌËË ÂÁÂ͈ËË ·˚ÎÓ ÏÂÌ 1 ÒÏ, Ë Û ÚÂı, Û ÍÓÚÓ˚ı ˝ÚÓ ‡ÒÒÚÓflÌË ·˚ÎÓ ·ÓΠ1 ÒÏ [18, 20, 60]. ç‡ Ò„ӉÌfl¯ÌËÈ ‰Â̸ ÚÓθÍÓ ÂÁÂ͈Ëfl Ô˜ÂÌË ‚ Ó·˙ÂÏ R0 fl‚ÎflÂÚÒfl ‡‰Ë͇θÌÓÈ. ìÏÂ̸¯ÂÌË ÓÔÛıÓ΂ÓÈ Ï‡ÒÒ˚ Ò ÔÓÏÓ˘¸˛ Ô‡ÎΡÚË‚ÌÓÈ ÂÁÂ͈ËË (Ó·˙ÂÏ R1) Ì ÛÎÛ˜¯‡ÂÚ ÔÓ„ÌÓÁ ÔÓ Ò‡‚ÌÂÌ˲ Ò ÒËÏÔÚÓχÚ˘ÂÒÍÓÈ Ú‡ÔËÂÈ [24]. 2. óËÒÎÓ ÏÂÚ‡ÒÚ‡ÁÓ‚. ç‡Î˘Ë 3 Ë ·ÓΠÏÂÚ‡ÒÚ‡ÁÓ‚, ‡ Ú‡ÍÊ ·ËÎÓ·‡ÌÓ ÔÓ‡ÊÂÌË Á̇˜ËÚÂθÌÓ ÛıÛ‰¯‡˛Ú ÔÓ„ÌÓÁ (Ú‡·Î. 2), ÌÓ, ÌÂÒÏÓÚfl ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 Ô˜Â̸ ÇéêéÅúÖÇ Ë ‰. 퇷Îˈ‡ 3. ŇÎθ̇fl ÒËÒÚÂχ ÓˆÂÌÍË ÔÓ„ÌÓÁ‡ èÓ„ÌÓÒÚ˘ÂÒÍËÈ Ù‡ÍÚÓ Å‡ÎÎ˚ èÓ‡ÒÚ‡ÌË ÒÂÓÁÌÓÈ Ó·ÓÎÓ˜ÍË Ô‚˘ÌÓÈ ÓÔÛıÓθ˛ 1 èÓ‡ÊÂÌË ÎËÏÙ‡Ú˘ÂÒÍËı ÛÁÎÓ‚ 1 èÂËÓ‰ ÓÚ Û‰‡ÎÂÌËfl Ô‚˘ÌÓÈ ÓÔÛıÓÎË ‰Ó ‚˚fl‚ÎÂÌËfl ÏÂÚ‡ÒÚ‡ÁÓ‚ ÏÂÌ 2 ÎÂÚ 1 óËÒÚÓ ÏÂÚ‡ÒÚ‡ÁÓ‚ ·ÓΠ3 1 è‰ÓÔ‡ˆËÓÌÌ˚È ÛÓ‚Â̸ êùÄ: 5–30 ÏÍ„/Î 1 ·ÓΠ30 ÏÍ„/Î 2 ê‡ÒÒÚÓflÌË ÓÚ Í‡fl ÏÂÚ‡ÒÚ‡Á‡ ‰Ó ÎËÌËË ÂÁÂ͈ËË ÏÂÌ 1 ÒÏ 1 ̇ ˝ÚÓ, ‚ ̇ÒÚÓfl˘Â ‚ÂÏfl ·Óθ¯ËÌÒÚ‚Ó ‡‚ÚÓÓ‚ Ì ҘËÚ‡˛Ú ̇΢ˠÏÌÓÊÂÒÚ‚ÂÌÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ (·ÓΠ4) ÔÓÚË‚ÓÔÓ͇Á‡ÌËÂÏ Í ÂÁÂ͈ËË ÔË ‚ÓÁÏÓÊÌÓÒÚË ‚˚ÔÓÎÌÂÌËfl  ‚ Ó·˙ÂÏ R0 [32, 33, 44, 60, 70]. ãËÏËÚËÛ˛˘ËÏ Ù‡ÍÚÓÓÏ ‚ ‰‡ÌÌÓÏ ÒÎÛ˜‡Â fl‚ÎflÂÚÒfl ÚÓθÍÓ ÌÂÓ·ıÓ‰ËÏÓÒÚ¸ Û‰‡ÎÂÌËfl ·ÓΠ70% Ô‡ÂÌıËÏ˚ Ô˜ÂÌË. 3. ÇÌÂÔ˜ÂÌÓ˜Ì˚ ÏÂÚ‡ÒÚ‡Á˚ ÛıÛ‰¯‡˛Ú ÔÓ„ÌÓÁ. é‰Ì‡ÍÓ Ì‡Î˘Ë ÂÁÂÍÚ‡·ÂθÌ˚ı ‚ÌÂÔ˜ÂÌÓ˜Ì˚ı ÔÓ‡ÊÂÌËÈ (·Û‰¸ ÚÓ ÂˆË‰Ë‚ Ô‚˘ÌÓÈ ÓÔÛıÓÎË ËÎË ÏÂÚ‡ÒÚ‡Á˚ ‚ ΄ÍËÂ) Ì fl‚ÎflÂÚÒfl ÔÓÚË‚ÓÔÓ͇Á‡ÌËÂÏ Í ıËۄ˘ÂÒÍÓÏÛ Î˜ÂÌ˲, ÔÓÁ‚ÓÎfl˛˘ÂÏÛ ‰ÓÒÚË„ÌÛÚ¸ 5-ÎÂÚÌÂÈ ‚˚ÊË‚‡ÂÏÓÒÚË Ì ÏÂÌ 25% [40]. ÑÎfl Ò‡‚ÌÂÌËfl: ÒÂ‰Ë Ô‡ˆËÂÌÚÓ‚ Ò ÌÂÂÁÂÍÚ‡·ÂθÌ˚ÏË ‚ÌÂÔ˜ÂÌÓ˜Ì˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË 2-, 3- Ë 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÒÓÒÚ‡‚Îfl˛Ú 36, 11% Ë 0 ÒÓÓÚ‚ÂÚÒÚ‚ÂÌÌÓ [8]. 4. ÇÂÏfl ÔÓfl‚ÎÂÌËfl ÏÂÚ‡ÒÚ‡ÁÓ‚. èÓ„ÌÓÁ Û Ô‡ˆËÂÌÚÓ‚ Ò ÏÂÚ‡ıÓÌÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË ÎÛ˜¯Â, ˜ÂÏ Û Ô‡ˆËÂÌÚÓ‚ Ò ÒËÌıÓÌÌ˚ÏË. èÓ ‰‡ÌÌ˚Ï K. Hughes Ë ÒÓ‡‚Ú. [32], ÔË ‚˚fl‚ÎÂÌËË ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍÓ„Ó ÔÓ‡ÊÂÌËfl Ô˜ÂÌË ·ÓΠ˜ÂÏ ˜ÂÂÁ 1 „Ó‰ ÔÓÒΠۉ‡ÎÂÌËfl Ô‚˘ÌÓÈ ÓÔÛıÓÎË 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÔÓÒΠÂÁÂ͈ËË ÒÓÒÚ‡‚ÎflÂÚ 42%, ÂÒÎË Ê ÏÂÚ‡ÒÚ‡Á˚ ӷ̇ÛÊÂÌ˚ ÏÂÌ ˜ÂÏ ˜ÂÂÁ 1 „Ó‰ ÔÓÒΠۉ‡ÎÂÌËfl Ô‚˘ÌÓ„Ó Ó˜‡„‡ – 24%. Ä̇Îӄ˘Ì˚ ÂÁÛθڇÚ˚ ÔÓÎÛ˜ÂÌ˚ ‰Û„ËÏË ‡‚ÚÓ‡ÏË [21, 59, 70]. 5. ìÓ‚Â̸ ‡ÍÓ‚Ó-˝Ï·ËÓ̇θÌÓ„Ó ‡ÌÚË„Â̇ ‚ Ô‰ÓÔ‡ˆËÓÌÌÓÏ ÔÂËӉ ‚˚¯Â 200 Ì„/ÏÎ fl‚Îfl- ÂÚÒfl Ì··„ÓÔËflÚÌ˚Ï Ù‡ÍÚÓÓÏ ÔÓ„ÌÓÁ‡ [21, 29, 68]. ÇÓÁ‡ÒÚ Ë ÔÓÎ Ô‡ˆËÂÌÚ‡, ÔÓ ‰‡ÌÌ˚Ï ÎËÚ‡ÚÛ˚, ‰ÓÒÚÓ‚ÂÌ˚ÏË Ù‡ÍÚÓ‡ÏË ÔÓ„ÌÓÁ‡ Ì fl‚Îfl˛ÚÒfl. è‰ÔÓÎÓÊÂÌËÂ Ó ‚ÎËflÌËË ‡Áχ ÓÔÛıÓÎË Ì‡ ÔÓ„ÌÓÁ [20] Ì ÔӉڂ‰ËÎÓÒ¸, Ë ˝ÚÓÚ Ù‡ÍÚÓ Ì ‰ÓÎÊÂÌ ‚ÎËflÚ¸ ̇ ÔËÌflÚË ¯ÂÌËfl Ó Ôӂ‰ÂÌËË ÓÔ‡ˆËË [60]. î‡ÌˆÛÁÒÍÓÈ ıËۄ˘ÂÒÍÓÈ ‡ÒÒӈˇˆËÂÈ ·˚ÎÓ Ôӂ‰ÂÌÓ ËÒÒΉӂ‡ÌË 1568 Ô‡ˆËÂÌÚÓ‚, ÍÓÚÓ˚Ï ‚˚ÔÓÎÌflÎËÒ¸ ÓÔ‡ˆËË Ì‡ Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚. ç‡ ÓÒÌÓ‚‡ÌËË ÔÓÎÛ˜ÂÌÌ˚ı ÂÁÛθڇÚÓ‚ ·˚· ÒÓÁ‰‡Ì‡ ÒËÒÚÂχ ·‡ÎθÌÓÈ ÓˆÂÌÍË ÔÓ„ÌÓÁ‡ [48] (Ú‡·Î. 3). ì Ô‡ˆËÂÌÚÓ‚, Ëϲ˘Ëı 1–2 ·‡Î·, ‚ÂÓflÚÌÓÒÚ¸ ˆˉ˂‡ Á‡·Ó΂‡ÌËfl Ì‚˚ÒÓ͇ Ë ÓÊˉ‡Âχfl 2-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÒÓÒÚ‡‚ÎflÂÚ ÓÍÓÎÓ 80%. ë Û‚Â΢ÂÌËÂÏ ÍÓ΢ÂÒÚ‚‡ ·‡ÎÎÓ‚ ÛıÛ‰¯‡ÂÚÒfl ÔÓ„ÌÓÁ: ÔË Ì‡Î˘ËË 5 ·‡ÎÎÓ‚ Ë ·ÓΠ2-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ì Ô‚˚¯‡ÂÚ 35%. çÂÓ·ıÓ‰ËÏÓ ÔÓÏÌËÚ¸, ˜ÚÓ ÚÓθÍÓ ‚ 20% ̇·Î˛‰ÂÌËÈ ÏÂÚ‡ÒÚ‡Á˚ fl‚Îfl˛ÚÒfl ÂÁÂÍÚ‡·ÂθÌ˚ÏË ‚ ÏÓÏÂÌÚ ÛÒÚ‡ÌÓ‚ÎÂÌËfl ‰Ë‡„ÌÓÁ‡ [39], ÔÓ˝ÚÓÏÛ ·Óθ¯ËÌÒÚ‚Ó ËÒÒΉӂ‡ÌËÈ ‡ÍˆÂÌÚËÓ‚‡ÌÓ Ì‡ ÔÓËÒÍ ÒÔÓÒÓ·Ó‚ ÔÓ‚˚¯ÂÌËfl ÂÁÂÍÚ‡·ÂθÌÓÒÚË Ë Ô‰ÛÔÂʉÂÌËfl ˆˉ˂ËÓ‚‡ÌËfl ÏÂÚ‡ÒÚ‡ÁÓ‚ Í‡Í ‚ Ò‡ÏÓÈ Ô˜ÂÌË, Ú‡Í Ë ‚ ‰Û„Ëı Ó„‡Ì‡ı. ê‡Á‡·ÓÚ‡ÌÌ˚ ÏÂÚÓ‰˚ ÏÓ„ÛÚ ÔËÏÂÌflÚ¸Òfl Í‡Í Ò‡ÏÓÒÚÓflÚÂθÌÓ, Ú‡Í Ë ‚ ÍÓÏ·Ë̇ˆËË, ‡ Ú‡ÍÊ fl‚ÎflÚ¸Òfl ‰ÓÔÓÎÌÂÌËÂÏ Í ÂÁÂ͈ËË Ô˜ÂÌË, ÒÓÒÚ‡‚Îflfl, Ú‡ÍËÏ Ó·‡ÁÓÏ, ÓÒÌÓ‚Û ÍÓ̈ÂÔˆËË ÍÓÏ·ËÌËÓ‚‡ÌÌÓ„Ó ÔÓ‰ıÓ‰‡ Í Î˜ÂÌ˲ ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË. èÓ‚ÚÓÌ˚ ÂÁÂ͈ËË. êˆˉ˂˚ ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍÓ„Ó ÔÓ‡ÊÂÌËfl Ô˜ÂÌË ‡Á‚Ë‚‡˛ÚÒfl Û 14–61% Ô‡ˆËÂÌÚÓ‚ ÔÓÒΠԂ˘ÌÓÈ ÂÁÂ͈ËË, Ô˘ÂÏ ÚÓθÍÓ Û 15–25% ÓÌË Ó„‡Ì˘ÂÌ˚ Ô˜Â̸˛ [15, 31, 70]. ì Ô‡ˆËÂÌÚÓ‚ ˝ÚÓÈ „ÛÔÔ˚ ‚ÓÁÏÓÊÌÓ ‚˚ÔÓÎÌÂÌË ÔÓ‚ÚÓÌ˚ı ÂÁÂ͈ËÈ, ÍÓÚÓ˚ ËÏÂ˛Ú Ô‡ÍÚ˘ÂÒÍË Ú‡ÍÓÈ Ê ÔÓ„ÌÓÁ, Í‡Í Ô‚‡fl ÂÁÂ͈Ëfl, ˜ÚÓ ‰Â·ÂÚ ÓÔ‡‚‰‡ÌÌ˚Ï Ëı ‚˚ÔÓÎÌÂÌË [65] (Ú‡·Î. 4). ç‰ÍÓ ÔË ÎÓ͇ÎËÁ‡ˆËË ÏÂÚ‡ÒÚ‡ÁÓ‚ ‚ Ô‡‚ÓÈ ‰ÓΠӄ‡Ì˘˂‡˛˘ËÏ ÂÁÂÍÚ‡·ÂθÌÓÒÚ¸ Ù‡ÍÚÓÓÏ fl‚ÎflÂÚÒfl χÎ˚È Ó·˙ÂÏ Ô‡ÂÌıËÏ˚ ΂ÓÈ ‰ÓÎË, ÓÒÚ‡˛˘ÂÈÒfl ÔÓÒΠÂÁÂ͈ËË. ë ˆÂθ˛ Û‚Â΢ÂÌËfl ÂÁ‚ӂ ΂ÓÈ ‰ÓÎË Ô˜ÂÌË Á‡ Ò˜ÂÚ ÍÓÏÔÂÌÒ‡ÚÓÌÓÈ „ËÔÂÚÓÙËË Ô‰ÎÓÊÂÌÓ ‚˚ÔÓÎÌÂÌË Ô‰ ÓÔ‡ˆËÂÈ ˝Ï·ÓÎËÁ‡ˆËË ËÎË Ô‚flÁÍË Ô‡‚ÓÈ í‡·Îˈ‡ 4. èflÚËÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÔË ÔÓ‚ÚÓÌ˚ı ÂÁÂ͈Ëflı Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÂˆË‰Ë‚Ì˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË ÉÓ‰ óËÒÎÓ ÓÔ‡ˆËÈ íÂıÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸, % èflÚËÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ % K. Riesenger Ë ÒÓ‡‚Ú. [55] 1996 25 53 36 S. Bines Ë ÒÓ‡‚Ú. [12] 1996 13 – 23 R. Adam Ë ÒÓ‡‚Ú. [5] 1997 63 60 41 Ä‚ÚÓ˚ ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà 7 ÚÓÏ 9 ‹1 2004 97 Ô˜Â̸ ãÖóÖçàÖ åÖíÄëíÄáéÇ èÖóÖçà äéãéêÖäíÄãúçéâ ùíàéãéÉàà ‚ÂÚ‚Ë ‚ÓÓÚÌÓÈ ‚ÂÌ˚. ùÚÓ ‚ϯ‡ÚÂθÒÚ‚Ó ÏÓÊÂÚ ·˚Ú¸ ÔÓËÁ‚‰ÂÌÓ ıËۄ˘ÂÒÍËÏ, ·ԇÓÒÍÓÔ˘ÂÒÍËÏ Ë ˜ÂÒÍÓÊÌ˚Ï ÒÔÓÒÓ·ÓÏ. ìÊ ˜ÂÂÁ 2 ̉ ÔÓÒΠÔӈ‰Û˚ ÔÓËÒıÓ‰ËÚ Û‚Â΢ÂÌË ӷ˙Âχ ΂ÓÈ ‰ÓÎË ‚ Ò‰ÌÂÏ ‚ 1.5 ‡Á‡ ÓÚ ËÒıÓ‰ÌÓ„Ó [10]. èË ·ËÎÓ·‡ÌÓÏ ÔÓ‡ÊÂÌËË ‚ÓÁÏÓÊÌÓ Ôӂ‰ÂÌË ‰‚Ûı˝Ú‡ÔÌÓÈ ÂÁÂ͈ËË Ô˜ÂÌË: Ô‚˚Ï ˝Ú‡ÔÓÏ Û‰‡Îfl˛Ú Ó‰ÌÛ ‰Óβ Ò ÛÁ·ÏË, ‚ÚÓ˚Ï, ÔÓÒΠ‡Á‚ËÚËfl „ËÔÂÚÓÙËË ÓÒÚ‡‚¯ÂÈÒfl ‰ÓÎË, ‚˚ÔÓÎÌfl˛Ú ÎË·Ó Ò„ÏÂÌÚ‡ÌÛ˛ ÂÁÂÍˆË˛, ÎË·Ó ÎÓ͇θÌÛ˛ ‰ÂÒÚÛÍˆË˛ ÛÁÎÓ‚ [6]. ïËÏËÓÚ‡ÔËfl, ‡ÒÒχÚË‚‡‚¯‡flÒfl ‡ÌÂÂ Í‡Í Â‰ËÌÒÚ‚ÂÌÌ˚È ÏÂÚÓ‰ ΘÂÌËfl ÌÂÂÁÂÍÚ‡·ÂθÌ˚ı ÔÓ‡ÊÂÌËÈ Ô˜ÂÌË, Ú‡ÍÊ ̇ıÓ‰ËÚ ÏÂÒÚÓ ÒÂ‰Ë ÏÂÚÓ‰Ó‚ ÍÓÏ·ËÌËÓ‚‡ÌÌÓ„Ó Î˜ÂÌËfl ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚. çÂÓ‡‰˙˛‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl. èÓ‚˚ÒËÚ¸ ÂÁÂÍÚ‡·ÂθÌÓÒÚ¸ Ô˜ÂÌÓ˜Ì˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚, ‡ Ú‡ÍÊ ‚ÓÁ‰ÂÈÒÚ‚Ó‚‡Ú¸ ̇ ÏËÍÓÏÂÚ‡ÒÚ‡Á˚ Ô˚Ú‡˛ÚÒfl ÔÛÚÂÏ Ôӂ‰ÂÌËfl ÌÂÓ‡‰˙˛‚‡ÌÚÌÓÈ ıËÏËÓÚ‡ÔËË. R. Adam Ë ÒÓ‡‚Ú. [7] ÒÓÓ·˘‡˛Ú Ó Ôӂ‰ÂÌËË ÌÂÓ‡‰˙˛‚‡ÌÚÌÓÈ ıËÏËÓÚ‡ÔËË 701 Ô‡ˆËÂÌÚÛ Ò ÌÂÂÁÂÍÚ‡·ÂθÌ˚ÏË ÍÓÎÓÂÍڇθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË ‚ Ô˜Â̸. ì 13.6% Ô‡ˆËÂÌÚÓ‚ ·˚Î ÓÚϘÂÌ ÔÂÂıÓ‰ ÏÂÚ‡ÒÚ‡ÁÓ‚ ‚ ÂÁÂÍÚ‡·ÂθÌÓ ÒÓÒÚÓflÌËÂ. ùÚË Ô‡ˆËÂÌÚ˚ ·˚ÎË ÓÔÂËÓ‚‡Ì˚, 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÒÓÒÚ‡‚Ë· 34%, ˜ÚÓ ÒÓÔÓÒÚ‡‚ËÏÓ Ò ÂÁÛθڇڇÏË Ô‚˘Ì˚ı ÂÁÂ͈ËÈ. Ç ˆÂÎÓÏ ‡‚ÚÓ‡Ï Û‰‡ÎÓÒ¸ ÔÓ‚˚ÒËÚ¸ ÂÁÂÍÚ‡·ÂθÌÓÒÚ¸ Ò 20 ‰Ó 30%. ĉ˙˛‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl. ñËÍÛÎËÛ˛˘Ë ‚ ÍÓ‚Ë ÓÔÛıÓ΂˚ ÍÎÂÚÍË Ó·Ì‡ÛÊË‚‡˛Ú Û 40% ·ÓθÌ˚ı ÍÓÎÓÂÍڇθÌ˚Ï ‡ÍÓÏ [67]. äÓÏ ÚÓ„Ó, ‚˚Ò‚Ó·Óʉ‡˛˘ËÂÒfl ÔÓÒΠÂÁÂ͈ËË Ô˜ÂÌË Ù‡ÍÚÓ˚ ÓÒÚ‡ ÒÚËÏÛÎËÛ˛Ú Ì ÚÓθÍÓ ‰ÂÎÂÌË ÌÓχθÌ˚ı „ÂÔ‡ÚÓˆËÚÓ‚, ÌÓ Ë ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ [51, 53]. ùÚÓ fl‚ÎflÂÚÒfl Ó·ÓÒÌÓ‚‡ÌËÂÏ ÌÂÓ·ıÓ‰ËÏÓÒÚË ËÒÔÓθÁÓ‚‡ÌËfl ‡‰˙˛‚‡ÌÚÌÓ„Ó Î˜ÂÌËfl ÔÓÒΠ‡‰Ë͇θÌ˚ı ıËۄ˘ÂÒÍËı ÓÔ‡ˆËÈ Ì‡ Ô˜ÂÌË [3, 9, 67]. çÂψÍË ËÒÒΉӂ‡ÚÂÎË ÔÓ͇Á‡ÎË, ˜ÚÓ Ôӂ‰ÂÌË ‡‰˙˛‚‡ÌÚÌÓÈ ıËÏËÓÚ‡ÔËË ÒÌËʇÂÚ ËÒÍ ÒÏÂÚË ÓÚ ÔÓ„ÂÒÒËÓ‚‡ÌËfl Á‡·Ó΂‡ÌËfl Ì ÏÂÌ ˜ÂÏ Ì‡ 15% [41]. ÇÓÁÏÓÊÌ˚ ‡Á΢Ì˚ ÒÔÓÒÓ·˚ ‚‚‰ÂÌËfl ıËÏËÓÔÂÔ‡‡ÚÓ‚ ‚ Ó„‡ÌËÁÏ: ÒËÒÚÂÏÌÓÂ, ‚ÌÛÚˇÚ¡θÌÓÂ, ‚ÌÛÚËÔÓڇθÌÓÂ Ë ËÌÚ‡ÔÂËÚÓ̇θÌÓÂ. ïÓÚfl ÓÔÚËχθÌ˚È ÏÂÚÓ‰ ¢ ÓÍÓ̘‡ÚÂθÌÓ Ì ÓÔ‰ÂÎÂÌ [42], ÌÂÍÓÚÓ˚ ËÒÒΉӂ‡ÚÂÎË ‰ÂÏÓÌÒÚËÛ˛Ú ÔÂËÏÛ˘ÂÒÚ‚Ó ‚ÌÛÚˇÚ¡θÌÓ„Ó ‚‚‰ÂÌËfl, ÒÓÁ‰‡˛˘Â„Ó ·ÓΠ‚˚ÒÓÍÛ˛ ÍÓ̈ÂÌÚ‡ˆË˛ ıËÏËÓÔÂÔ‡‡Ú‡ ‚ ÓÔÛıÓÎË Ë ÒÌËʇ˛˘Â„Ó Â„Ó ÒËÒÚÂÏÌÓ ÚÓÍÒ˘ÂÒÍÓ ‰ÂÈÒÚ‚ËÂ. í‡Í, N. Kemeny Ë ÒÓ‡‚Ú. [36] ‚˚fl‚ËÎË Û‚Â΢ÂÌË ÍÓ΢ÂÒÚ‚‡ ·ÓθÌ˚ı ·ÂÁ ˆˉ˂ӂ ‚ Ú˜ÂÌË 2 ÎÂÚ ÔÓÒΠÂÁÂ͈ËË Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ò 60 ‰Ó 90% ÔË ‚ÌÛÚˇÚ¡θÌÓÈ ıËÏËÓÚ‡ÔËË ÔÓ Ò‡‚ÌÂÌ˲ Ò ÒËÒÚÂÏÌÓÈ. Ç Í‡˜ÂÒÚ‚Â ÏÂÚÓ‰ËÍ, ÔÓ‚˚¯‡˛˘Ëı ˝ÙÙÂÍÚË‚ÌÓÒÚ¸ ‚ÓÁ‰ÂÈÒÚ‚Ëfl ıËÏËÓÔÂÔ‡‡Ú‡ ̇ ÓÔÛıÓ΂˚ ÍÎÂÚÍË, ‡ÒÒχÚË‚‡˛Ú ÏÂÚÓ‰ ıËÏËÓ˝Ï·ÓÎËÁ‡ˆËË 98 Ô˜ÂÌÓ˜ÌÓÈ ‡ÚÂËË, Ó·ÂÒÔ˜˂‡˛˘ËÈ ÒÂÎÂÍÚË‚ÌÓ ̇ÍÓÔÎÂÌË ıËÏËÓÔÂÔ‡‡Ú‡ ‚ ÓÔÛıÓÎË Ë ‚˚Á˚‚‡˛˘ËÈ Ë¯ÂÏ˘ÂÒÍËÈ ÌÂÍÓÁ ÌÓ‚ÓÓ·‡ÁÓ‚‡ÌËfl, ÛÒËÎË‚‡˛˘ËÈ Ú‡Ô‚Ú˘ÂÒÍËÈ ˝ÙÙÂÍÚ ·ÂÁ Á̇˜ËÚÂθÌÓ„Ó ÔÓ‚ÂʉÂÌËfl ÌÓχθÌÓÈ Ô‡ÂÌıËÏ˚ [1]. éÒÌÓ‚Ì˚ ÓÒÎÓÊÌÂÌËfl ıËÏËÓ˝Ï·ÓÎËÁ‡ˆËË (3–4%): Ô˜ÂÌӘ̇fl ̉ÓÒÚ‡ÚÓ˜ÌÓÒÚ¸ ËÎË ËÌÙ‡ÍÚ˚ Ô˜ÂÌË, Ô˜ÂÌÓ˜Ì˚ ‡·ÒˆÂÒÒ˚, ·ËΡÌ˚ ÌÂÍÓÁ˚, ‡Á˚‚ ÓÔÛıÓÎË, ıÓΈËÒÚËÚ, ÌÂÍÓÌÚÓÎËÛÂχfl ˝Ï·ÓÎËÁ‡ˆËfl ÒÓÒÛ‰Ó‚ ÊÂÎۉ͇ Ë/ËÎË Í˯˜ÌË͇; ÎÂڇθÌÓÒÚ¸ ‚‡¸ËÛÂÚ ÓÚ 1 ‰Ó 4% [37, 58, 64]. ïËÏËÓ˝Ï·ÓÎËÁ‡ˆËfl ‚ ÓÒÌÓ‚ÌÓÏ ‡ÒÒχÚË‚‡ÂÚÒfl ‚ ͇˜ÂÒÚ‚Â ÔÓÒΉÌÂ„Ó ËÁ ÏÂÚÓ‰Ó‚ ΘÂÌËfl ·ÓθÌ˚ı Ò ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍËÏ ÔÓ‡ÊÂÌËÂÏ Ô˜ÂÌË, Û ÍÓÚÓ˚ı Ô‰¯ÂÒÚ‚Û˛˘‡fl ÒËÒÚÂÏ̇fl Ë/ËÎË Â„ËÓ̇θ̇fl ıËÏËÓÚ‡ÔËfl ·˚· ̽ÙÙÂÍÚË‚ÌÓÈ. ëÚ‡·ËÎËÁ‡ˆËfl ËÎË ˜‡ÒÚ˘̇fl „ÂÒÒËfl ÓÔÛıÓ΂˚ı Ó˜‡„Ó‚ ÓÚϘÂ̇ Û 59–72% ·ÓθÌ˚ı, ‚ 17% ̇·Î˛‰ÂÌËÈ ÓÚ˜‡Î‡Ò¸ ÔÓÎ̇fl „ÂÒÒËfl. ÄÍÚۇ̇fl 1- Ë 2-„Ӊ˘̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÒÓÒÚ‡‚Ë· ÒÓÓÚ‚ÂÚÒÚ‚ÂÌÌÓ 68–86% Ë 37–55%. å‰ˇ̇ ‚˚ÊË‚‡ÂÏÓÒÚË ÔÓÒΠԂÓÈ ıËÏËÓ˝Ï·ÓÎËÁ‡ˆËË ÒÓÒÚ‡‚Ë· 8–10 ÏÂÒ [37, 58, 64]. ãÓ͇θ̇fl ‰ÂÒÚÛ͈Ëfl ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍËı ÛÁÎÓ‚. èÓÔ˚ÚÍË ÎÓ͇θÌÓ„Ó ‡ÁÛ¯ÂÌËfl ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô‰ÔËÌËχÎËÒ¸ ‰‡‚ÌÓ. é‰ÌËÏ ËÁ Ô‚˚ı Ë Ì‡Ë·ÓΠÔÓÒÚ˚ı ÏÂÚÓ‰Ó‚ ·˚ÎÓ ÔËÏÂÌÂÌË ˝Ú‡ÌÓÎÓ‚Ó„Ó ÒÔËÚ‡. ǂ‰ÂÌË ˝Ú‡ÌÓ·. ùÚ‡ ÏÂÚÓ‰Ë͇ ÓÒÌÓ‚‡Ì‡ ̇ ‚‚‰ÂÌËË ‚ ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍËÈ ÛÁÂÎ (ËÌÚ‡ÓÔ‡ˆËÓÌÌÓ ËÎË ˜ÂÒÍÓÊÌÓ) ÔÓ‰ ÍÓÌÚÓÎÂÏ ìáà 96% ÒÔËÚ‡. åÂÚÓ‰ ‚Ò ¢ ËÒÔÓθÁÛÂÚÒfl ÔË Î˜ÂÌËË ÌÂÂÁÂÍÚ‡·ÂθÌ˚ı ÓÔÛıÓÎÂÈ Ô˜ÂÌË, ˜ÚÓ Ó·ÛÒÎÓ‚ÎÂÌÓ Â„Ó ÓÚÌÓÒËÚÂθÌÓÈ ÔÓÒÚÓÚÓÈ Ë ‰Â¯Â‚ËÁÌÓÈ. èË ˝ÚÓÏ 3-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ÒÓÒÚ‡‚ÎflÂÚ ‰Ó 39% [58]. Ç ˝ÍÒÔÂËÏÂÌÚ ·˚ÎÓ ÔÓ͇Á‡ÌÓ, ˜ÚÓ ÌÂÔÓÎ̇fl ‰ÂÒÚÛ͈Ëfl ÓÔÛıÓÎÂ‚Ó„Ó ÛÁ· ÔÓËÒıÓ‰ËÚ ‚ 89% ÒÎÛ˜‡Â‚ [26]. ǂ‰ÂÌË ÒÔËÚ‡ ÏÓÊÂÚ fl‚ÎflÚ¸Òfl ‡Î¸ÚÂ̇ÚË‚Ì˚Ï ÏÂÚÓ‰ÓÏ Î˜ÂÌËfl Ì·Óθ¯Ëı ÌÂÂÁÂÍÚ‡·ÂθÌ˚ı ÓÔÛıÓÎÂÈ, Ӊ̇ÍÓ Â„Ó Ì ÒΉÛÂÚ ÂÍÓÏẨӂ‡Ú¸ ÔË Î˜ÂÌËË ·ÓΠÍÛÔÌ˚ı ÓÔÛıÓÎÂÈ ËÁ-Á‡ ÚÂıÌ˘ÂÒÍËı ÒÎÓÊÌÓÒÚÂÈ, Ò‚flÁ‡ÌÌ˚ı Ò Ôӈ‰ÛÓÈ ËÌ˙Â͈ËË, ‡ Ú‡ÍÊ ËÁ-Á‡ ÌÂÛ‰Ó‚ÎÂÚ‚ÓËÚÂθÌ˚ı ÓÚ‰‡ÎÂÌÌ˚ı ÂÁÛθڇÚÓ‚ Ë Ì‚ÓÁÏÓÊÌÓÒÚË ÍÓÌÚÓÎËÓ‚‡Ú¸ Ó·˙ÂÏ ‡ÁÛ¯‡ÂÏÓÈ Ú͇ÌË. Ç ÔÓÒΉÌË 3–5 ÎÂÚ ˝Ú‡ ÏÂÚÓ‰Ë͇ Òڇ· ÛÒÚÛÔ‡Ú¸ ÏÂÒÚÓ ·ÓΠÔÓ„ÂÒÒË‚Ì˚Ï Ë ˝ÙÙÂÍÚË‚Ì˚Ï ÏÂÚÓ‰‡Ï – ‡‰ËÓ˜‡ÒÚÓÚÌÓÈ ‡·Î‡ˆËË (‰ÂÒÚÛ͈ËË, êóÄ) Ë ÍËÓ‰ÂÒÚÛ͈ËË. ꇉËÓ˜‡ÒÚÓÚ̇fl ‰ÂÒÚÛ͈Ëfl (‡·Î‡ˆËfl – êóÄ). ùÚÓÚ ÏÂÚÓ‰ Ô‰ÒÚ‡‚ÎflÂÚ ÒÓ·ÓÈ Ì‡„‚‡ÌË Ú͇ÌÂÈ ‚ÓÍÛ„ ÒÔˆˇθÌÓ„Ó ˝ÎÂÍÚÓ‰‡ ÔÓ„ÛÊÂÌÌÓ„Ó ‚ ÓÔÛıÓ΂˚È Ó˜‡„ ÔÓÒ‰ÒÚ‚ÓÏ ‡‰ËÓ‚ÓÎÌ ˜‡ÒÚÓÚÓÈ 450–500 ÍɈ, Ó·ÂÒÔ˜˂‡˛˘Ëı ̇„‚ ÓÍÛʇ˛˘Ëı Ú͇ÌÂÈ ‰Ó 80–110°ë, ˜ÚÓ ÔË‚Ó‰ËÚ Í ÍÓ‡„ÛÎflˆËÓÌÌÓÏÛ ÌÂÍÓÁÛ. èÓÒΉÌË ÏÓ‰ÂÎË ˝ÎÂÍÚÓ‰Ó‚ Ò ‚˚‰‚ËÊÌ˚ÏË Ë„Óθ˜‡Ú˚ÏË Í˛˜Í‡ÏË ÔÓÁ‚ÓÎfl˛Ú ÓÒÛ˘ÂÒÚ‚ÎflÚ¸ ÍÓ‡„ÛÎflˆË˛ Ó·‡ÁÓ‚‡ÌËÈ ‰Ë‡ÏÂÚÓÏ ‰Ó 7 ÒÏ. ó‡ÒÚÓÚ‡ ÓÒÎÓÊÌÂÌËÈ ÔÓÒΠêóÄ ÒÓÒÚ‡‚ÎflÂÚ 0–12 %, ÎÂڇθÌÓÒÚ¸ 0–1% ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 Ô˜Â̸ ÇéêéÅúÖÇ Ë ‰. 퇷Îˈ‡ 5. ùÙÙÂÍÚË‚ÌÓÒÚ¸ ÍËÓ‰ÂÒÚÛ͈ËË Ë ‡‰ËÓ˜‡ÒÚÓÚÌÓÈ ‰ÂÒÚÛ͈ËË ÌÂÂÁÂÍÚ‡·ÂθÌ˚ı ÓÔÛıÓÎÂÈ Ô˜ÂÌË [50] 臈ËÂÌÚ˚/ÏÂÚ‡ÒÚ‡Á˚ éÒÎÓÊÌÂÌËfl, % (p < 0.001) ëÓÍ Ì‡·Î˛‰ÂÌËfl, ÏÂÒ. êˆˉ˂, % (p < 0.001) äËÓ‰ÂÒÚÛ͈Ëfl 54/88 40.7 15 13.6 êóÄ 92/138 3.3 15 2.1 åÂÚÓ‰ [16, 69], ˆˉ˂˚ ‚ ÏÂÒÚ ‰ÂÒÚÛ͈ËË ‚ÓÁÌË͇˛Ú ‚ 6–18% ̇·Î˛‰ÂÌËÈ [54, 63]. äËÓ‰ÂÒÚÛ͈Ëfl. åÂÚÓ‰ Óı·ʉÂÌËfl ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ ‰Ó ÚÂÏÔ‡ÚÛ˚, ‚˚Á˚‚‡˛˘ÂÈ Ëı „Ë·Âθ. ó‡ÒÚÓÚ‡ ÓÒÎÓÊÌÂÌËÈ, Ò‚flÁ‡ÌÌ˚ı Ò ÍËÓ‰ÂÒÚÛ͈ËÂÈ, ‰Ó‚ÓθÌÓ ‚˚ÒÓ͇ (15–50%), ÎÂڇθÌÓÒÚ¸ ÓÍÓÎÓ 4%, ˜‡ÒÚÓÚ‡ ˆˉ˂ӂ ÒÓÒÚ‡‚ÎflÂÚ 10–15% [23, 52, 72]. ùÙÙÂÍÚË‚ÌÓÒÚ¸ ÍËÓ‰ÂÒÚÛ͈ËË Ë ‡‰ËÓ˜‡ÒÚÓÚÌÓÈ „ËÔÂÚÂÏËË ÔË Î˜ÂÌËË Ô‡ˆËÂÌÚÓ‚ Ò ÌÂÂÁÂÍÚ‡·ÂθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË Ô˜ÂÌË Ô˂‰Â̇ ‚ Ú‡·Î. 5. ä ÌÓ‚˚Ï ÏÂÚÓ‰‡Ï ÎÓ͇θÌÓÈ ‰ÂÒÚÛ͈ËË ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍËı ÛÁÎÓ‚ Ô˜ÂÌË, ̇ıÓ‰fl˘ËÏÒfl ‚ ÒÚ‡‰ËË ËÁÛ˜ÂÌËfl Ë Ì ÔÓÎۘ˂¯ËÏ ÔÓ͇ ¯ËÓÍÓ„Ó ‡ÒÔÓÒÚ‡ÌÂÌËfl ‚ ÍÎËÌ˘ÂÒÍÓÈ Ô‡ÍÚËÍÂ, ÏÓÊÌÓ ÓÚÌÂÒÚË ÏËÍÓ‚ÓÎÌÓ‚Û˛ Ë ËÌÚÂÒÚˈˇθÌÛ˛ ·ÁÂÌÛ˛ ÍÓ‡„ÛÎflˆË˛. åËÍÓ‚ÓÎÌÓ‚‡fl ÍÓ‡„ÛÎflˆËfl. Ç ÓÒÌÓ‚Â ÏÂÚÓ‰‡ ÎÂÊËÚ ‚˚ÒÓÍÓ˜‡ÒÚÓÚÌÓ ËÁÎÛ˜ÂÌË (˜‡ÒÚÓÚ‡ ‰Ó 2450 åɈ), ‚˚Á˚‚‡˛˘Â „ËÔÂÚÂÏ˘ÂÒÍÓ ‡ÁÛ¯ÂÌË ÓÔÛıÓ΂˚ı Ó˜‡„Ó‚ ‰Ë‡ÏÂÚÓÏ ‰Ó 3 ÒÏ. ÑÎfl ˝ÚÓ„Ó ÒÔˆˇθÌ˚È ‡ÔÔÎË͇ÚÓ ‚‚Ó‰flÚ ‚ ÛÁÂÎ ÎË·Ó ˜ÂÒÍÓÊÌÓ, ÎË·Ó ËÌÚ‡ÓÔ‡ˆËÓÌÌÓ. èÓÎÌ˚È ÌÂÍÓÁ ÓÔÛıÓ΂ÓÈ Ú͇ÌË ‰ÓÒÚË„‡˛Ú Û 72% Ô‡ˆËÂÌÚÓ‚ [30, 43]. éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ÔËÏÂÌÂÌËfl ˝ÚÓ„Ó ÏÂÚÓ‰‡ ÒÓÔÓÒÚ‡‚ËÏ˚ Ò ÂÁÛθڇڇÏË ‡‰ËÓ˜‡ÒÚÓÚÌÓÈ „ËÔÂÚÂÏ˘ÂÒÍÓÈ ‰ÂÒÚÛ͈ËË [25]. àÌÚÂÒÚˈˇθ̇fl ·ÁÂ̇fl ÚÂÏÓ‰ÂÒÚÛ͈Ëfl. ã‡ÁÂÌÓ ËÁÎÛ˜ÂÌË ÔÓ‰‡ÂÚÒfl Í ÓÔÛıÓÎË ÔÓ ÒÔˆˇθÌÓÏÛ Ò‚ÂÚÓ‚ÓÎÓÍÌÛ. Ç Ú͇ÌË ˝ÚÓ ËÁÎÛ˜ÂÌË ÔÂÓ·‡ÁÛÂÚÒfl ‚ ÚÂÔÎÓ‚Û˛ ˝Ì„˲. ÑˇÏÂÚ ‡ÁÛ¯‡ÂÏ˚ı Ó˜‡„Ó‚ ‚ Á‡‚ËÒËÏÓÒÚË ÓÚ ÏÓ˘ÌÓÒÚË „Â̇ÚÓ‡ Ë ÚËÔ‡ ÔÓ‚Ó‰fl˘Ëı ‚ÓÎÓÍÓÌ ÒÓÒÚ‡‚ÎflÂÚ ÓÚ 2 ‰Ó 8 ÒÏ [30, 45]. ìÒËÎËflÏË ‰‚Ûı ωˈËÌÒÍËı Û˜ÂʉÂÌËÈ (Éçñä åËÌÁ‰‡‚‡ êî Ë êçñï êÄåç) ̇˜‡Ú‡ ‰Ó΄ÓÒӘ̇fl ÍÓÏÔÎÂÍÒ̇fl ÔÓ„‡Ïχ ÔÓ ËÁÛ˜ÂÌ˲ ‚ÓÁÏÓÊÌÓÒÚÂÈ ÒÓ‚ÂÏÂÌÌ˚ı ÏÂÚÓ‰Ó‚ ΘÂÌËfl ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË. чθÌÂȯ ‡Á‚ËÚË ˝ÚÓ„Ó Ì‡Ô‡‚ÎÂÌËfl ÓÒÌÓ‚˚‚‡ÎÓÒ¸ ̇ ÛÊ Ëϲ˘ÂÏÒfl ÓÔ˚ڠΘÂÌËfl ˝ÚÓÈ „ÛÔÔ˚ Ô‡ˆËÂÌÚÓ‚. ë ÒÂÌÚfl·fl 2001 „. ÔÓ Ï‡Ú 2003 „. ·˚ÎÓ ‚˚ÔÓÎÌÂÌÓ 28 ÂÁÂ͈ËÈ Ô˜ÂÌË ÔÓ ÔÓ‚Ó‰Û ÒËÌıÓÌÌ˚ı (9/32%) Ë ÏÂÚ‡ıÓÌÌ˚ı (19/68%) ÍÓÎÓÂÍڇθÌ˚ı ÏÂÚ‡ÒÚ‡ÁÓ‚. ë‰ÌËÈ ‚ÓÁ‡ÒÚ Ô‡ˆËÂÌÚÓ‚ ÒÓÒÚ‡‚ËÎ 56.4 ± 9.7 „Ó‰‡ (42–73 „Ó‰‡), ÏÛʘËÌ ·˚ÎÓ 12, ÊÂÌ˘ËÌ – 16 (ÒÓÓÚÌÓ¯ÂÌË 1 : 1.3). èÓ͇Á‡ÌËfl Í ‚˚ÔÓÎÌÂÌ˲ ÓÔ‡ˆËË Ì‡ Ô˜ÂÌË ÓÔ‰ÂÎflÎË ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ÚÓθÍÓ ÔÓÒΠ‡‰Ë͇θÌÓ„Ó Û‰‡ÎÂÌËfl Ô‚˘ÌÓÈ ÓÔÛıÓÎË. Ç 75% ̇·Î˛‰ÂÌËÈ ËÒÚÓ˜ÌËÍÓÏ ÏÂÚ‡ÒÚ‡ÁËÓ‚‡ÌËfl ·˚· ÓÔÛıÓθ ÔflÏÓÈ Í˯ÍË, ‚ 18% – Ó·Ó‰Ó˜ÌÓÈ, ‚ 7% – ÒË„ÏӂˉÌÓÈ. åÂÚ‡ıÓÌÌ˚ ÏÂÚ‡ÒÚ‡Á˚ ‚˚fl‚ÎflÎË ‚ Ò‰ÌÂÏ ˜ÂÂÁ 19.7 ± 9.1 ÏÂÒ (7–31 ÏÂÒ) ÔÓÒΠۉ‡ÎÂÌËfl Ô‚˘ÌÓÈ ÓÔÛıÓÎË Í˯ÍË. ÑÎfl ‰Ë‡„ÌÓÒÚËÍË ÔÓ‡ÊÂÌËfl Ô˜ÂÌË ËÒÔÓθÁÓ‚‡ÎË ìáà Ó„‡ÌÓ‚ ·˛¯ÌÓÈ ÔÓÎÓÒÚË, äí, ÒÔˇθÌÛ˛ äí Ò ‚ÌÛÚË‚ÂÌÌ˚Ï ÍÓÌÚ‡ÒÚËÓ‚‡ÌËÂÏ, åêí, ·ԇÓÒÍÓÔ˲. èË Ó·¯ËÌÓÏ ÔÓ‡ÊÂÌËË Ë Ì·Óθ¯ÓÈ Î‚ÓÈ ‰ÓΠ‡ÒÒ˜ËÚ˚‚‡ÎË ÚÓ˜Ì˚È Ó·˙ÂÏ ‰ÓÎÂÈ Ô˜ÂÌË Ì‡ ÓÒÌÓ‚‡ÌËË äí-ÂÍÓÌÒÚÛ͈ËË. èÓ‡ÊÂÌˠ΂ÓÈ ‰ÓÎË ‚˚fl‚ÎÂÌÓ Û 7 (25%) Ô‡ˆËÂÌÚÓ‚, Ô‡‚ÓÈ – Û 9 (31%), Ó·ÂËı ‰ÓÎÂÈ – Û 12 (44%). óËÒÎÓ ÏÂÚ‡ÒÚ‡ÁÓ‚ ‚‡¸ËÓ‚‡ÎÓ ÓÚ 1 ‰Ó 5. ëÓÎËÚ‡Ì˚È ÏÂÚ‡ÒÚ‡Á ËÏÂÎÒfl Û 44% ·ÓθÌ˚ı, 2 ÏÂÚ‡ÒÚ‡Á‡ – Û 12%, 3 ÏÂÚ‡ÒÚ‡Á‡ Ë ·ÓΠ– Û 44% ·ÓθÌ˚ı. ÑˇÏÂÚ Ò‡Ï˚ı ÍÛÔÌ˚ı ÛÁÎÓ‚ ÍÓη‡ÎÒfl ÓÚ 2 ‰Ó 10 ÒÏ (‚ Ò‰ÌÂÏ 5.7 ± 2.7 ÒÏ). Ç˚ÔÓÎÌÂÌ˚ ÒÎÂ‰Û˛˘Ë ÓÔ‡ˆËË: 14 Ô‡‚ÓÒÚÓÓÌÌËı „ÂÏË„ÂÔ‡Ú˝ÍÚÓÏËÈ (ÉÉù) (ËÁ ÌËı 2 ‡Ò¯ËÂÌÌ˚Â), 5 ΂ÓÒÚÓÓÌÌËı (‚ ÚÓÏ ˜ËÒΠ2 ‡Ò¯ËÂÌÌ˚Â) Ë 9 ·Ú‡θÌ˚ı ΂ÓÒÚÓÓÌÌËı ÂÁÂ͈ËÈ Ô˜ÂÌË. èË ‰ËÒÒÂ͈ËË Ô‡ÂÌıËÏ˚ Ô˜ÂÌË Û 11 Ô‡ˆËÂÌÚÓ‚ ËÒÔÓθÁÓ‚‡ÎË ‚Ó‰ÓÒÚÛÈÌ˚È ‰ËÒÒÂÍÚÓ (“Helix-HydroJet”), ‰Îfl ‰ÓÒÚËÊÂÌËfl ÓÍÓ̘‡ÚÂθÌÓ„Ó „ÂÏÓÒÚ‡Á‡ ‡Ì‚ÓÈ ÔÓ‚ÂıÌÓÒÚË Ô˜ÂÌË Û 17 ËÁ 28 ·ÓθÌ˚ı ÔËÏÂÌflÎË ÙË·ËÌ-ÍÓη„ÂÌÓ‚Û˛ ÒÛ·ÒÚ‡ÌˆË˛. ì 10 Ô‡ˆËÂÌÚÓ‚ ÔËÏÂÌÂ̇ ÚÂıÌÓÎÓ„Ëfl êóÄ ÏÂÚ‡ÒÚ‡ÁÓ‚ (RITA Medical Systems, Inc, Model 1500): ‚ 6 ̇·Î˛‰ÂÌËflı ‚Ó ‚ÂÏfl Ô‡‚ÓÒÚÓÓÌÌÂÈ ÉÉù, ‚ 2 – ÔË Î‚ÓÒÚÓÓÌÌÂÈ ÉÉù Ë ‚ 2 – ÔË ·ËÎÓ·‡ÌÓÏ ÔÓ‡ÊÂÌËË Ô˜ÂÌË Í‡Í Ò‡ÏÓÒÚÓflÚÂθÌ˚È ÏÂÚÓ‰. ÑË̇Ï˘ÂÒÍÓ ̇·Î˛‰ÂÌË Á‡ ÁÓ̇ÏË ‡‰ËÓ˜‡ÒÚÓÚÌÓ„Ó ‚ÓÁ‰ÂÈÒÚ‚Ëfl ÔÓ‚Ó‰ËÎË Ò ÔÓÏÓ˘¸˛ ìáà Ë äí, ÍÓÚÓ˚ ÔÓ‚ÚÓflÎË ˜ÂÂÁ 1 ̉ Ë 1 ÏÂÒ ÔÓÒΠÓÔ‡ˆËË. ì 2 Ô‡ˆËÂÌÚÓ‚ êóÄ ÔÓ‚Ó‰ËÎË ‚ÚÓ˚Ï ˝Ú‡ÔÓÏ ˜ÂÂÁ 2.5 Ë 3 ÏÂÒ ÔÓÒΠÂÁÂ͈ËË Ô˜ÂÌË ÒÓÓÚ‚ÂÚÒÚ‚ÂÌÌÓ, ̇ ÙÓÌ ‡Á‚Ë‚¯ÂÈÒfl ÍÓÏÔÂÌÒ‡ÚÓÌÓÈ „ËÔÂÚÓÙËË ÓÒÚ‡‚¯ÂÈÒfl ‰ÓÎË Ô˜ÂÌË. êÂÁÛθڇÚ˚ àÌÚ‡ÓÔ‡ˆËÓÌÌÓÈ Ë „ÓÒÔËڇθÌÓÈ ÎÂڇθÌÓÒÚË ÔÓÒΠ‚˚ÔÓÎÌÂÌÌ˚ı ‚ϯ‡ÚÂθÒÚ‚ Ì ÓÚϘÂÌÓ. ë‰Ìflfl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÓÔ‡ˆËË ÒÓÒÚ‡‚Ë· 335 ± 90 ÏËÌ. (180–490 ÏËÌ.), ÓÔ‡ˆËÓÌ̇fl ÍÓ‚ÓÔÓÚÂfl – 943 ± 578 ÏÎ (250–2250 ÏÎ). èÓÒÎÂÓÔ‡ˆËÓÌÌ˚ ÓÒÎÓÊÌÂÌËfl ÓÚϘÂÌ˚ Û 8 (28.6%) Ô‡ˆËÂÌÚÓ‚: Ô˜ÂÌӘ̇fl ̉ÓÒÚ‡ÚÓ˜‹1 2004 99 7* Ô˜Â̸ ãÖóÖçàÖ åÖíÄëíÄáéÇ èÖóÖçà äéãéêÖäíÄãúçéâ ùíàéãéÉàà åÂÚ‡ÒÚ‡Á˚ Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË êÂÁÂÍÚ‡·ÂθÌ˚ çÂÓ‡‰˙‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl??? ìÒÎÓ‚ÌÓ ÂÁÂÍÚ‡·ÂθÌ˚ çÂÓ‡‰˙‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl ùÏ·ÓÎËÁ‡ˆËfl, Ô‚flÁ͇ Ô‡‚ÓÈ ‚ÂÚ‚Ë ‚ÓÓÚÌÓÈ ‚ÂÌ˚ çÂÂÁÂÍÚ‡·ÂθÌ˚ ãÓ͇θ̇fl ‰ÂÒÚÛ͈Ëfl (êóÄ, ÍËÓ‰ÂÒÚÛ͈Ëfl Ë ‰.) ïËÏËÓÚ‡ÔËfl (ÒËÒÚÂÏ̇fl, ‚ÌÛÚˇÚ¡θ̇fl çÂÚ ˝ÙÙÂÍÚ‡ êÂÁÂ͈Ëfl Ô˜ÂÌË êÂÁÂÍÚ‡·ÂθÌÓ çÂÂÁÂÍÚ‡·ÂθÌÓ ïËÏËÓ˝Ï·ÓÎËÁ‡ˆËfl ‚ÂÚ‚Ë Ô˜ÂÌÓ˜ÌÓÈ ‡ÚÂËË Ä‰˙˛‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl ãÓ͇θ̇fl ‰ÂÒÚÛ͈Ëfl (êóÄ, ÍËÓ‰ÂÒÚÛ͈Ëfl) Ä΄ÓËÚÏ ÍÓÏ·ËÌËÓ‚‡ÌÌÓ„Ó Î˜ÂÌËfl ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË. ÌÓÒÚ¸ – 1, ̇ÛÊÌ˚È ÊÂΘÌ˚È Ò‚Ë˘ – 2, Òԇ˜̇fl Í˯˜̇fl ÌÂÔÓıÓ‰ËÏÓÒÚ¸ – 1, ÔÓ‰‰Ë‡Ù‡„χθÌÓ ÊˉÍÓÒÚÌÓ ÒÍÓÔÎÂÌËÂ, ÔÓÚ·ӂ‡‚¯Â ˜ÂÒÍÓÊÌÓÈ ÔÛÌ͈ËË ÔÓ‰ ÛθڇÁ‚ÛÍÓ‚˚Ï ÍÓÌÚÓÎÂÏ – 4, ̇„ÌÓÂÌË ÔÓÒÎÂÓÔ‡ˆËÓÌÌÓÈ ‡Ì˚ – 1. ëÂ‰Ë Ô‡ˆËÂÌÚÓ‚, Û ÍÓÚÓ˚ı ‚Ó ‚ÂÏfl ÓÔ‡ˆËË ÔËÏÂÌflÎË ‚Ó‰ÓÒÚÛÈÌ˚È ‰ËÒÒÂÍÚÓ Ë “í‡ıÓäÓÏ·” ÓÒÎÓÊÌÂÌËÈ, Ò‚flÁ‡ÌÌ˚ı Ò Ì‰ÓÒÚ‡ÚÓ˜Ì˚Ï „ÂÏÓÒÚ‡ÁÓÏ Ë Ì„ÂÏÂÚ˘ÌÓÒÚ¸˛ ÊÂΘÌ˚ı ÔÓÚÓÍÓ‚ ‡Ì‚ÓÈ ÔÓ‚ÂıÌÓÒÚË ÍÛθÚË Ô˜ÂÌË, Ì ÓÚϘÂÌÓ. ꇉËÓ˜‡ÒÚÓÚÌÓÈ ‰ÂÒÚÛ͈ËË ÔÓÒΠ‚˚ÔÓÎÌÂÌËfl ÂÁÂ͈ËË ÔÓ‰‚„‡ÎË Ó˜‡„Ë ‚ ÓÒÚ‡˛˘ÂÈÒfl ÍÛθÚ Ô˜ÂÌË. ë‰ÌËÈ ‰Ë‡ÏÂÚ ÏÂÚ‡ÒÚ‡Á‡ ÒÓÒÚ‡‚ËÎ 2.5 ± 1.2 ÒÏ. ì 2 Ô‡ˆËÂÌÚÓ‚ ÔË Ô‡‚ÓÒÚÓÓÌÌÂÏ Ë ˆÂÌڇθÌÓÏ ‡ÒÔÓÎÓÊÂÌËË ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍËı ÛÁÎÓ‚ Ë Ï‡ÎÓÈ Ï‡ÒҠ΂ÓÈ ‰ÓÎË êóÄ ÔËÏÂÌËÎË ·ÂÁ ÂÁÂ͈ËË Ô˜ÂÌË, ÔË ˝ÚÓÏ Ò‰ÌËÈ ‰Ë‡ÏÂÚ ÛÁÎÓ‚ ÒÓÒÚ‡‚ËÎ 3.2 ± 0.9 ÒÏ. Ñ‚Ûı˝Ú‡ÔÌÓ ‚ÓÁ‰ÂÈÒÚ‚Ë ̇ Ó‰ËÌ Ë ÚÓÚ Ê Ә‡„ Ò ¯‡„ÓÏ 1 ÒÏ (Ò ˆÂθ˛ ‡Ò¯ËÂÌËfl ÁÓÌ˚ ‰ÂÒÚÛ͈ËË) ÔËÏÂÌÂÌÓ Û 4 ·ÓθÌ˚ı. èÓÒΠêóÄ ÔË ËÌÚ‡ÓÔ‡ˆËÓÌÌÓÏ ìáà ‚Ó ‚ÒÂı ̇·Î˛‰ÂÌËflı ÓÚϘ‡ÎË ÔÂ͇˘ÂÌË ÍÓ‚ÓÚÓ͇ Ë Û‚Â΢ÂÌË ˝ıÓ„ÂÌÌÓÒÚË Ò ÔËÁ͇̇ÏË „ËÔÂÂÏËË Ô‡ÂÌıËÏ˚ Ô˜ÂÌË, ‡ÒÔÓÎÓÊÂÌÌÓÈ ÔÓ ÔÂËÙÂËË ÁÓÌ˚ ‰ÂÒÚÛ͈ËË. ìáà ˜ÂÂÁ 1 ̉. ÔÓÒΠÓÔ‡ˆËË Ôӂ‰ÂÌ˚ ‚ÒÂÏ ·ÓθÌ˚Ï. ìáà Ë äí ˜ÂÂÁ 1 ÏÂÒ ÔÓÒΠÓÔ‡ˆËË ‚˚ÔÓÎÌÂÌ˚ 5 Ô‡ˆËÂÌÚ‡Ï. èË ÍÓÌÚÓθÌ˚ı ìáà Ë äí Û‚Â΢ÂÌËfl ‰Ë‡ÏÂÚ‡ ÛÁÎÓ‚ Ë ÔËÁ̇ÍÓ‚ ÔÓfl‚ÎÂÌËfl ÍÓ‚ÓÚÓ͇ ‚ 100 ÁÓ̇ı ‰ÂÒÚÛ͈ËË Ì ÓÚϘ‡ÎÓÒ¸. ïËۄ˘ÂÒÍËı ÓÒÎÓÊÌÂÌËÈ, Ò‚flÁ‡ÌÌ˚ı Ò êóÄ, ÔÓÒΠÓÔ‡ˆËÈ Ì ·˚ÎÓ. 4 Ô‡ˆËÂÌÚ‡Ï ‚ ÒÓÓÚ‚ÂÚÒÚ‚ËË Ò ‡Á‡·ÓÚ‡ÌÌ˚Ï ÔÓÚÓÍÓÎÓÏ Ô‰ ÓÔ‡ˆËÂÈ ÔÓ‚Ó‰ËÎË ÌÂÓ‡‰˙˛‚‡ÌÚÌÛ˛ Ú‡Ô˲. èÓÒΉÌË 10 Ô‡ˆËÂÌÚÓ‚ ÔÓÎÛ˜‡ÎË ‡‰˙˛‚‡ÌÚÌÛ˛ ıËÏËÓÚ‡Ô˲ (5-ÙÚÓÛ‡ˆËÎ, ÎÂÈÍÓ‚‡ËÌ). Ñ‚ÛÏ Ô‡ˆËÂÌÚ‡Ï Ò ÏÌÓÊÂÒÚ‚ÂÌÌ˚ÏË ·ËÎÓ·‡Ì˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË ‚Ó ‚ÂÏfl ÓÔ‡ˆËË ÛÒÚ‡ÌÓ‚ÎÂÌ ËÌÚ‡‡Ú¡θÌ˚È ÔÓÚ ‰Îfl Ôӂ‰ÂÌËfl „ËÓ̇θÌÓÈ ıËÏËÓÚ‡ÔËË. Çϯ‡ÚÂθÒÚ‚Ó ÔÓ¯ÎÓ ·ÂÁ ÓÒÎÓÊÌÂÌËÈ. í‡ÍËÏ Ó·‡ÁÓÏ, ÏÂÚÓ‰ÓÏ ‚˚·Ó‡ ÔË Î˜ÂÌËË ÏÂÚ‡ÒÚ‡ÁÓ‚ Ô˜ÂÌË ÍÓÎÓÂÍڇθÌÓÈ ˝ÚËÓÎÓ„ËË ·˚· Ë ÓÒÚ‡ÂÚÒfl ÂÁÂ͈Ëfl Ô˜ÂÌË. ëÓ‚ÂÏÂÌÌ˚ ÏÂÚÓ‰˚ ΘÂÌËfl ÔÓÁ‚ÓÎfl˛Ú ‡ÒÒχÚË‚‡Ú¸ ‡Ì ӉÌÓÁ̇˜ÌÓ ÌÂÓÔ‡·ÂθÌ˚ı ·ÓθÌ˚ı Í‡Í ÔÓÚÂ̈ˇθÌÓ ÓÔ‡·ÂθÌ˚ı. èÓ‚˚¯ÂÌ˲ ÂÁÂÍÚ‡·ÂθÌÓÒÚË ÏÓÊÂÚ ÒÔÓÒÓ·ÒÚ‚Ó‚‡Ú¸ Ôӂ‰ÂÌË ÌÂÓ‡‰˙˛‚‡ÌÚÌÓÈ ıËÏËÓÚ‡ÔËË. èË “ÔÓ·ÎÂÏÌÓÈ” (χÎÓÈ) ΂ÓÈ ‰ÓΠ‚ÓÁÏÓÊÌÓ ‚˚ÔÓÎÌÂÌË ˝Ï·ÓÎËÁ‡ˆËË ËÎË Ô‚flÁÍË Ô‡‚ÓÈ ‚ÂÚ‚Ë ‚ÓÓÚÌÓÈ ‚ÂÌ˚, ÒÔÓÒÓ·ÒÚ‚Û˛˘ÂÈ ÍÓÏÔÂÌÒ‡ÚÓÌÓÈ „ËÔÂÚÓÙËË Î‚ÓÈ ‰ÓÎË. ë ˆÂθ˛ ÔÓÙË·ÍÚËÍË ‰‡Î¸ÌÂÈ¯Â„Ó ÏÂÚ‡ÒÚ‡ÁËÓ‚‡ÌËfl ÔÓ͇Á‡ÌÓ Ôӂ‰ÂÌË ‡‰˙˛‚‡ÌÚÌÓÈ Ú‡ÔËË ÔÓÒΠÂÁÂ͈ËË Ô˜ÂÌË. èÂÒÔÂÍÚË‚Ì˚Ï Ì‡Ô‡‚ÎÂÌËÂÏ ÏÓÊÌÓ Ò˜ËÚ‡Ú¸ ËÒÔÓθÁÓ‚‡ÌË „ËÓ̇θÌÓÈ ‚ÌÛÚˇÚ¡θÌÓÈ ıËÏËÓÚ‡ÔËË, ÓÒÓ·ÂÌÌÓ ‚ ÒÓ˜ÂÚ‡ÌËË Ò ÂÁÂ͈ËÂÈ Ô˜ÂÌË, ÎË·Ó Ò ÎÓ͇θÌ˚Ï ‡ÁÛ¯ÂÌËÂÏ ÏÂ- ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 Ô˜Â̸ ÇéêéÅúÖÇ Ë ‰. Ú‡ÒÚ‡ÁÓ‚. ïËÏËÓ˝Ï·ÓÎËÁ‡ˆËfl ‚ÂÚ‚ÂÈ Ô˜ÂÌÓ˜ÌÓÈ ‡ÚÂËË fl‚ÎflÂÚÒfl “ÏÂÚÓ‰ÓÏ ÓÚ˜‡flÌËfl” Ë ÏÓÊÂÚ ‚˚ÔÓÎÌflÚ¸Òfl ÔË Ì½ÙÙÂÍÚË‚ÌÓÒÚË Ì‡Á‚‡ÌÌ˚ı ‚˚¯Â ÏÂÓÔËflÚËÈ. ãÓ͇θÌÛ˛ ‰ÂÒÚÛÍˆË˛ (êóÄ, ÍËÓ‰ÂÒÚÛ͈Ëfl Ë ‰.) ˆÂÎÂÒÓÓ·‡ÁÌÓ ÔËÏÂÌflÚ¸ Í‡Í ‰ÓÔÓÎÌÂÌËÂ Í ÂÁÂ͈ËË Ô˜ÂÌË ÔË ÏÌÓÊÂÒÚ‚ÂÌÌ˚ı, ÓÒÓ·ÂÌÌÓ ·ËÎÓ·‡Ì˚ı, ÏÂÚ‡ÒÚ‡Á‡ı ËÎË Í‡Í Ò‡ÏÓÒÚÓflÚÂθÌ˚È ÏÂÚÓ‰ ÔË Ó‰ÌÓÁ̇˜ÌÓ ÌÂÂÁÂÍÚ‡·ÂθÌ˚ı ÏÂÚ‡ÒÚ‡Á‡ı (ÒÏ. ËÒÛÌÓÍ). á‡Íβ˜ÂÌË åÌÓ„ÓÓ·‡ÁËÂ Ë ÌÂÒڇ̉‡ÚÌÓÒÚ¸ ÍÎËÌ˘ÂÒÍËı ÔÓfl‚ÎÂÌËÈ ÔÓ‡ÊÂÌËfl Ô˜ÂÌË ÍÓÎÓÂÍڇθÌ˚ÏË ÏÂÚ‡ÒÚ‡Á‡ÏË Ì‰ÍÓ Ú·ÛÂÚ Ë̉˂ˉۇθÌÓ„Ó ÔÓ‰ıÓ‰‡ Í ‚˚·ÓÛ Ú‡ÍÚËÍË Î˜ÂÌËfl Ë ÔËÏÂÌÂÌËfl ÍÓÏ·Ë̇ˆËË ‡Á΢Ì˚ı ÏÂÚÓ‰Ó‚ (ÂÁÂ͈Ëfl, ÎÓ͇θ̇fl ‰ÂÒÚÛ͈Ëfl ÛÁÎÓ‚, ‡Á΢Ì˚ ÂÊËÏ˚ ıËÏËÓÚ‡ÔËË Ë ‰.). ç‡ÍÓÔÎÂÌÌ˚È ÓÔ˚Ú Á‡Û·ÂÊÌ˚ı ÍÓÎ΄ Ë Ì‡¯ ̇˜‡Î¸Ì˚È ÍÎËÌ˘ÂÒÍËÈ ÓÔ˚Ú ÔÓ͇Á˚‚‡˛Ú, ˜ÚÓ ÍÓÏ·ËÌËÓ‚‡ÌÌ˚È ÔÓ‰ıÓ‰ Í Î˜ÂÌ˲ ˝ÚÓÈ „ÛÔÔ˚ ·ÓθÌ˚ı ÏÓÊÂÚ ËÒÔÓθÁÓ‚‡Ú¸Òfl ‰ÓÒÚ‡ÚÓ˜ÌÓ ·ÂÁÓÔ‡ÒÌÓ Ë ÒÓÔÓ‚Óʉ‡Ú¸Òfl ÌËÁÍÓÈ ÎÂڇθÌÓÒÚ¸˛ Ë ÔËÂÏÎÂÏ˚Ï ÛÓ‚ÌÂÏ ÓÒÎÓÊÌÂÌËÈ. ÑÎfl ÓÍÓ̘‡ÚÂθÌÓ„Ó Â¯ÂÌËfl Ú‡ÍÚ˘ÂÒÍËı ‚ÓÔÓÒÓ‚ Ë ÒÓÁ‰‡ÌËfl ‡Î„ÓËÚÏÓ‚ ΘÂÌËfl Ú‡ÍËı Ô‡ˆËÂÌÚÓ‚ Ú·ÛÂÚÒfl Ôӂ‰ÂÌË ‰‡Î¸ÌÂȯËı ÔÓÚÓÍÓθÌ˚ı ÏÛθÚˈÂÌÚÓ‚˚ı ËÒÒΉӂ‡ÌËÈ Ò ÓˆÂÌÍÓÈ ÓÚ‰‡ÎÂÌÌ˚ı ÂÁÛθڇÚÓ‚. ëÔËÒÓÍ ÎËÚ‡ÚÛ˚ 1. ɇÌÓ‚ Ä.å. Ò ÒÓ‡‚Ú. àÌÚ‚Â̈ËÓÌ̇fl ‡‰ËÓÎÓ„Ëfl ‚ ΘÂÌËË Ô‚˘ÌÓ„Ó Ë ÏÂÚ‡ÒÚ‡Ú˘ÂÒÍÓ„Ó ‡Í‡ Ô˜ÂÌË. ÇÂÒÚÌ. ÂÌÚ„ÂÌÓÎ. 1998. ‹ 1. ë. 48–52. 2. äÓÌ‚ Ç.É. ëÓ‚ÂÏÂÌÌ˚ ıËÏËÓÔÂÔ‡‡Ú˚ ‚ ΘÂÌËË ·ÓθÌ˚ı ÍÓÎÓÂÍڇθÌ˚Ï ‡ÍÓÏ Ò ÏÂÚ‡ÒÚ‡Á‡ÏË ‚ Ô˜Â̸. éÌÍÓÎÓ„Ëfl. 2002. 4. ‹ 1. ë. 62–65. 3. éÂÎ ç.î. ĉ˙˛‚‡ÌÚ̇fl ıËÏËÓÚ‡ÔËfl ÍÓÎÓÂÍڇθÌÓ„Ó ‡Í‡. êåÜ. 2002. 10. ‹ 14. 4. è‡Ú˛ÚÍÓ û.à. Ò ÒÓ‡‚Ú. ëÓ‚ÂÏÂÌÌ˚ ÔÓ‰ıÓ‰˚ Í ıËۄ˘ÂÒÍÓÏÛ Î˜ÂÌ˲ ÓÔÛıÓÎÂÈ Ô˜ÂÌË. ÇÓÔ. ÓÌÍÓÎÓ„ËË 1998. 44(5). ë. 580–583. 5. Adam R. et al. Repeat hepatectomy for colorectal liver metastases. Ann. Surg. 1997. 225. P. 51–62. 6. Adam R. et al. Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann. Surg. 2000 Dec. 232(6). P. 777–785. 7. Adam R. et al. Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal liver metastases. An. Surg. Onc. 2001. 8(4). P. 347–353. 8. Adson et al. Resection of hepatic metastases from colorectal cancer. Arch. Surg. 1984. 119. P. 647–651. 9. Alberts S.R. et al. Intrahepatic therapy for resected hepatic metastases from colorectal carcinoma. Oncology. 2000 Dec. 14(12). P. 48–51. 10. Barbaro B. et al. Preoperative right portal vein embolization in patients with metastatic liver disease. Metastatic liver volumes after RPVE. Acta. Radiol. 2003. Jan. 44(1). P. 98–102. ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 11. Bengtsson G. et al. Natural history of patients with untreated liver metastases from colorectal cancer. Am. J. Surg. 1981. 141. P. 586–589. 12. Bines S.D. et al. Survival after repeat hepatic resection for recurrent colorectal hepatic metastases. Surgery 1996 Oct. 120(4). P. 591–596. 13. Cady B. et al. The role of surgical resection of liver metastases in colorectal carcinoma. Semin. Onco. 1991. ‹ 18. P. 339–340. 14. Cervone A. et al. Intraoperative ultrasound (IOUS) is essential in the management of metastatic colorectal liver lesions. Am. Surg. 2000. Jul. 66(7). P. 611–615. 15. Chunningham J.D. et al. One hundred consecutive hepatic resections: blood loss, transfusion and opertiva technique. Arch. Surg. 1994. 129. P. 1050–1056. 16. Curley S.A., Izzo F., Curley S.A., Izzo F., Delrio P. et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies. Ann. Surg. 1999. ‹ 230. P. 1–8. 17. DeMatteo R. et al. Anatomi segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J. Gastrointest. Surg. 2000. 4. P. 178–184. 18. Elias D. et al. Resection of liver metastases from colorectal cancer: the real impact of the surgical margin. Eur. J. Surg. Oncol. 1998. 24. P. 174–179. 19. Elias D. et al. What are the real indications for hepatectomies in metastases of colorectal origin. Gastroenterol. Clin. Biol. 1998. Dec. 22(12). P. 1048–1055. 20. Fong Y. et al. Liver resection for colorectal metastases. J. Clin. Oncol. 1997. 15. P. 938–946. 21. Fong Y. et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann. Surg. 1999 Sep. 230(3). P. 309–318. 22. Fujii K. et al. Factors influencing survial in 33 patients undergoing resections of hepatic metastases from colorectal cancer.Hepatogastroenterology 2000 May-Jun. 47(33). P. 607–611. 23. Gagne D.J., Roh M.S. Cryosurgery for hepatic malignancies. In: Curley SA (ed). Liver cancer. New York: Springer-Verlag. 1998. P. 173–200. 24. Geoghegan J. et al. Treatment of colorectal liver metastases. Br. J. Surg. 1999. 86. P. 158–169. 25. Greve J.W. Alternative techniques for treatment of colon carcinoma metastases in liver: current status in the Netherlands. Scand. J. Gastroenterol Suppl. 2001. (234). P. 77–81. 26. Hahn P.F. et al. Liver tumor ablation: real time monitoring with dynamic CT. Acad. Radiol. 1997. Sep. 4(9). P. 634–638. 27. Hardy K.J. et al. One hundred liver resections including comparison to non-resected liver-mobilized patients. Aust. N. Z. J. Surg. 1998 Oct. 68(10). P. 716–721. 28. Harms et al. The role of surgery in the treatment of liver metastases for colorectal cancer patients. Hepatogastroenterology. 1999. 46. P. 2321–2328. 29. Heslin M.J. et al. Colorectal hepatic metastases: resection, local ablation, and hepatic artery infusion pump are assotiated with prolonged survival. Arch. Surg. 2001 Mar. 136(3). P. 318–323. ‹1 2004 101 Ô˜Â̸ ãÖóÖçàÖ åÖíÄëíÄáéÇ èÖóÖçà äéãéêÖäíÄãúçéâ ùíàéãéÉàà 30. Ho S.G.F. et al. Minimally invasive treatment of colorectal cancer metastases: current status and new directions. BC. Med. J. 2000. Dec. 42(10). P. 461–464. 31. Hohenberger P. et al. Tumor recurrence and options for further treatment after resection of liver metastases in patients with colorectal cancer. J. Surg. Oncol. 1990. 44. P. 245–251. 32. Hughes K.S. et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of patterns of recurrence. Surgery. 1989. 100. P. 278–284. 33. Iwatsuki S. et al. Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of prognostic scoring system. J. Am. Coll. Surg. 1999. 189. P. 291–299. 34. Jourdan J.L. et al. Hepatic resection for metastases in colorectal carcinoma. NZ Med J 1999 Mar 26. 112(1084). P. 91–93. 35. Kadry Z. et al. Treatment of primary and secondary liver malignancy. Swiss. Med. WKLY. 2001. 131. P. 338– 345. 36. Kemeny N. et al. Hepatic arterial infusion chemotherapy after resection of hepatic metastases from colorectal cancer. N. Engl. J. Med. 1999. 341. P. 2039–2048. 37. Lang E.K., Brown C.L., Jr. Colorectal metastases to the liver: selective chemoembolization. Radiology. 1993. 189. P. 417–422. 38. Lambert A. et al. Interval hepatic resection of colorectal metastases improves patient selection. Arch. Surg. 2000. 135. P. 473–480. 39. Largiader F.et al. Checkliste Chirurgie: Viszeral- und Allgemeinchirurgie - 7., voellig bearb. Und erw. Aufl. Stuttgart; New York: Thieme. 1998. P. 345. 40. Lehnert T. et al. Sequential hepatic and pulmonary resections for metastatic colorectal cancer. Br. J. Surg. 1999. 86. P. 784–788. 41. Lorenz M. et al. Randomized trial of surgery versus surgery followed by adjuvant hepatic arterial infusion with 5-fluorouracil and folinic acid for liver metastases of colorectal cancer. Ann. Surg. 1998. 228. P. 756–762. 42. Lorenz M. et al. Letter to the editor. N. Engl. J. Med. 2000. 342. P. 1524–1527. 43. Matsukava T. et al. Percutaneous microvawe coagulation therapy in liver tumors: a 3-year experience. Acta. Radiol. 1997. 38. P. 410–415. 44. Minagawa M. et al. Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal carcinoma: long-term results. Ann. Surg. 2000 Apr. 231(4). P. 487–499. 45. Muralidharan V. et al. Interstitial laser hyperthermia for colorectal liver metastases: the effect of thermal sensitization and the usr of a cylindrical diffuser tip on tumor necrosis. J. Clin. Laser. Med. Surg. 2002 Aug. 20(4). P. 189–196. 46. Teague B.D. et al. Electrolysis and other local ablative treatments for non-resectable colorectal liver metastases. ANZ. J. Surg. 2002 Feb. 72(2). 134–141. 47. Nadig D.E. et al. Major hepatic resection. Indications and results in a national system from 1988 to 1992. Arch. Surg. 1997 Feb. 132(2). P. 115–119. 48. Nordlinger B. et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. 102 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. Association Francaise de Chirurgie. Cancer. 1996. ‹ 77. P. 1254–1262. Ohlisson B. et al. Percutaneous fine-needle aspiration cytology in the diagnosis and management of liver tumors. Br. J. Surg. 2002 Jun. 89(6). P. 757–762. Pearson A.S. et al. Intraoperative radiofrequency ablation or cryoablation for hepatic malignances. Am. J. Surg. 1999 Dec. 178(6). P. 592–599. Picardo A. et al. Partial hepatectomy accelerates local tumor growth: potential roles of local cytokine aktivation. Surgery. 1998. 124. P. 57–64. Quebbeman E.J., Wallace J.R. Cryosurgery for hepatic metastases. In: Condon RE (ed). Current techniques in general surgery. New York: Mosby. 1997. P. 1–75. Rashidi B. et al. Minimal liver resection strongly stimulates the growth of human colon cancer in the liver of the nude mice. Clin Exp Metastasis. 1999. 17. P. 497–500. Rhim H., Dodd G.D. 3rd. Radiofrequency thermal ablation of liver tumors. J. Clin. Ultrasound. 1999. 5. P. 221– 229. Riesenger K.P. et al. Repeat resection of reccurent hepatic metastases – improvement in prognosis? Eur. J. Surg. 1996 Sep. 162(9). P. 709–715. Ruers T. et al. Treatment of liver metastases, an update on the possibilities and results. Eur. J. Cancer. 2002 May. 38(7). P. 1023–1033. Sanz-Altamira P.M., Spence L.D., Huberman M.S. et al. Selective chemoembolization in the management of hepatic metastases in refractory colorectal carcinoma: a phase II trial. Dis. Colon. Rectum. 40. P. 770–775, 1997. Sardi A. et al. Management of primary and metastatic tumors to the liver. Oncology. 1996. 10. Sasaki A. et al. Prognostic significance of intrahepatic lymphatic invasion in patients with hepatic resection due to metastases from colorectal carcinoma. Cancer. 2002 Jul. 1. 95(1). P. 105–111. Sheele J. et al. Indicators of prognosis after hepatic resection for colorectal secondaries. Surgery. 1991. ‹ 110. P. 13–29. Sheele J. et al. Resection of colorectal liver metastases. Langenbeck’s Arch. Surg. 1999. 384. P. 313–327. Shibata T., Niinobu T., Ogata N. Comparison of the effects of in-vivo thermal ablation of pig liver by microwave and radiofrequency coagulation. J Hepatobiliary Pancreat. Surg. 2000. 7. P. 592–598. Siperstein A. et al. Local recurrence after laparoscopic radiofrequency thermal ablation of hepatic tumors. Ann. Surg. Oncol. 2000. 7. P. 106–113. Tellez C., Benson A.B., 3rd, Lyster M.T. et al. Phase II trial of chemoembolization for the treatment of metastatic colorectal carcinoma to the liver and review of the literature. Cancer. 1998. 82. P. 1250–1259. Toccchi A. et al. Recurrent liver metastases from colorectal cancer: their surgical treatment. G. Chir. 1999 Jun-Jul. 20(6–7). P. 289–292. Shibata T. et al. Microwave coagulation therapy for multiple hepatic metastases from colorectal carcinoma. Cancer. 2000. Jul 15. 89(2). P. 276–284. Vogel I., Soeth E., Ruder C., et al. Disseminated tumor cells in the blood and/or bone marrow of patients with ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 Ô˜Â̸ ÇéêéÅúÖÇ Ë ‰. colorectal carcinoma are an independent prognostic factor. Ann. Oncol., 2000. 11 (suppl. 4). P. 43, abstr. 183. 68. Watine J. et al. Carcinoembryonic antigen as an independent prognostic factor of reccurence and survival in patients resected for colorectal liver metastases: a systematic review. Dis. Colon. Rectum. 2001. Dec. 44(22). P. 1791–1799. 69. Wood T.F., Rose D.M., Chung M. et al. Radiofrequency ablation of 231 unresectable hepatic tumours: indications, limitations and complications. Ann. Surg. Oncol. 2000. 7. P. 593–600. ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 70. Yamada H. et al. Analysis of predictive factors for recurrence after hepatectomy for colorectal liver metastases. World. J. Surg. 2001 Sep. 25(9). P. 1129–1133. 71. Yasui K. et al. Major anatomic hepatic resection with regional lymph node dissection for liver metastases from colorectal cancer. J. Hepatobiliary. Pancreat. Surg. 1995. 2. P. 103–106. 72. Yen K.A. et al. Cryosurgical ablation of hepatic metastases from colorectal carcinomas. Am. Surg. 1997. Jan. ‹ 63(1). P. 63–68. ‹1 2004 103