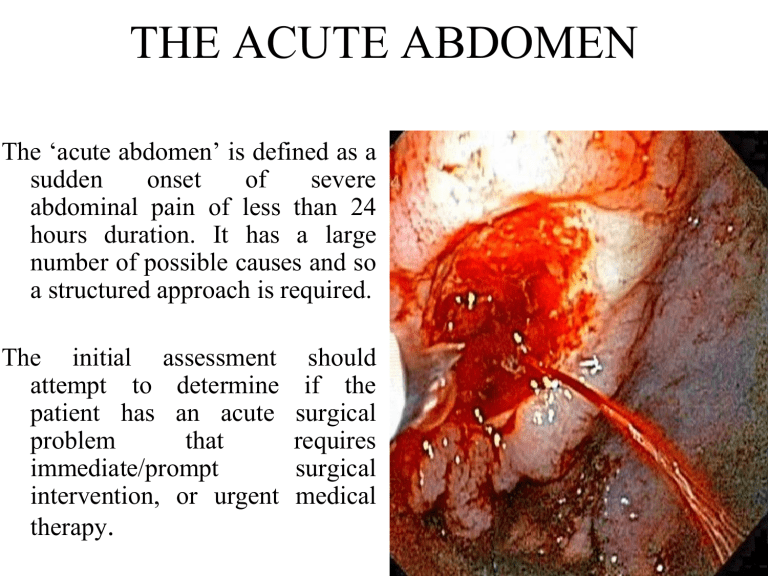
THE ACUTE ABDOMEN The ‘acute abdomen’ is defined as a sudden onset of severe abdominal pain of less than 24 hours duration. It has a large number of possible causes and so a structured approach is required. The initial assessment attempt to determine patient has an acute problem that immediate/prompt intervention, or urgent therapy. should if the surgical requires surgical medical THE ACUTE ABDOMEN • The ‘acute abdomen’ is defined as a medical condition, which is caused by acute destructive abdominal diseases. • These diseases have similar symptoms. • It is complicated by internal bleeding or peritonitis. • This condition requires emergency surgical intervention • Appendicitis • Acute cholecystitis • Acute pancreatitis • Peptic ulcer disease • Small bowel obstruction • Diverticulitis and other Сause of acute abdominal pain a group of acute destructive abdominal diseases that have similar symptoms and are complicated by peritonitis or bleeding and require surgical intervention • • • • • • • • • • • • • • Acute appendicitis. Acute peptic ulcer and its complications Acute cholecystitis Acute pancreatitis Acute intestinal ischemia (see section below) Acute diverticulitis Ectopic pregnancy with tubal rupture Ovarian torsion Acute peritonitis (including hollow viscus perforation) Bowel volvulus Bowel obstruction Abdominal aortic aneurysm Hemoperitoneum Ruptured spleen Peptic ulcer disease Other names Peptic ulcer, stomach ulcer, gastric ulcer, duodenal ulcer It should be noted that uncomplicated stomach ulcer does not belong to the category of acute abdomen. Only complications of gastric ulcer such as bleeding, perforation, penetration belong to the category of acute abdomen Symptom of free gas in the abdominal cavity Causes of small bowel obstruction include: [2] Adhesions from previous abdominal surgery (most common cause) Barbed sutures Pseudoobstruction Hernias containing bowel Crohn's disease causing adhesions or inflammatory strictures Neoplasms, benign or malignant Intussusception Volvulus Superior mesenteric artery syndrome, a compression of the duodenum by the superior mesenteric artery and the abdominal aorta Ischemic strictures Foreign bodies (e.g. gallstones in gallstone ileus, swallowed objects such as expandable water toys) Many women are not receiving the education needed from their doctors about adhesions. Very few women even know they have adhesions. Upright abdominal X-ray Abdominal X-rays Bowel obstruction Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction intestines which prevents the normal movement of the products of digestion small bowel or large bowel. Signs and symptoms include abdominal pain, vomiting, bloating (вздутие) and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital. Upright abdominal Xray demonstrating a small bowel obstruction. Note multiple air fluid levels. Diverticulitis Other names Colonic diverticulitis Section of large bowel (sigmoid colon) showing multiple pouches (diverticula). The diverticula appear on either side of the longitudinal muscle bundle (taenium) which runs horizontally across the specimen in an arc. Specialty General surgery Symptoms Abdominal pain, fever, nausea, diarrhea, constipation, blood in the stool Complications Abscess, fistula, bowel perforation Ectopic pregnancy Other names EP, eccyesis, extrauterine pregnancy, EUP, tubal pregnancy (when in fallopian tube) Laparoscopic view, looking down at the uterus (marked by blue arrows). In the left Fallopian tube there is an ectopic pregnancy and bleeding (marked by red arrows). The right tube is normal. Specialty Obstetrics and gynecology Symptoms Abdominal pain, vaginal bleeding[1] Risk factors Pelvic inflammatory disease, tobacco smoking, prior tubal surgery, history of infertility, use of assisted reproductive technology[2] Diagnostic method Blood tests for human chorionic gonadotropin (hCG), ultrasound[1] Differential diagnosis Miscarriage, ovarian torsion, acute appendicitis Treatment Methotrexate, surgery Prognosis Mortality 0.2% (developed world), 2% (developing world)[3] Frequency ~1.5% of pregnancies Ovarian torsion Other names Adnexal torsion Arteries of the female reproductive tract: uterine artery, ovarian artery and vaginal arteries. (Ovary and ovarian artery visible in upper right.) Specialty Gynecology Symptoms Pelvic pain Complications Infertility Usual onset Classically sudden Risk factors Ovarian cysts, ovarian enlargement, ovarian tumors, pregnancy, tubal ligation Diagnostic methodBased on symptoms, ultrasound, CT scan Differential diagnosis Appendicitis, kidney infection, kidney stones, ectopic pregnancy Treatment Surgery Frequency 6 per 100,000 women per year Peritonitis Peritonitis is an inflammation of the peritoneum, accompanied not only by local changes in the abdominal cover, but also by a severe general reaction of the body caused by intoxication, impaired intestinal function and vital organs. Peritonitis Other namesSurgical abdomen, acute abdomen Causes • • • • • • • Causes include: perforation of the intestinal tract, pancreatitis, pelvic inflammatory disease, stomach ulcer, or a ruptured appendix. Risk factors include ascites (the abnormal build-up of fluid in the abdomen) and peritoneal dialysis. Diagnosis is generally based on examination, blood tests, and medical imaging. • • • • • Physical examination In order to clinically examine a patient with an acute abdomen, it is necessary to: Inspection for injuries or hematomas, hernias, other abdominal wall defects or skin discoloration (pancreatitis). The stomach participates in the act of breathing Auscultation should always be performed prior to manual examination in order to avoid provoking intestinal noises. Intestinal sounds should be auscultated in 4 sections. Are there intestinal noises present? What grade are they? If no noises are heard, this could indicate a paralytic ileus. Palpation to detect muscle rigidity, muscle guarding, peritonism (rebound tenderness), tenderness, and ascites. Percussion helps in the detection of ascites, and abdominal fluid. Digital rectal examination for conditions such as palpable tumors, an empty bowel (caused by an obstacle such as ileus or tumor) and blood. Key symptoms of acute abdomen 1. Abdominal pain The main manifestations of peritonitis are acute abdominal pain, abdominal tenderness, abdominal guarding, rigidity, which are exacerbated by moving the peritoneum, e.g., coughing (forced cough may be used as a test), flexing one's hips, or eliciting the Blumberg sign (meaning that pressing a hand on the abdomen elicits less pain than releasing the hand abruptly, which will aggravate the pain, as the peritoneum snaps back into place). Rigidity is highly specific for diagnosing peritonitis (specificity: 76–100%). The presence of these signs in a person is sometimes referred to as peritonism. The localization of these manifestations depends on whether peritonitis is localized (e.g., appendicitis or diverticulitis before perforation), or generalized to the whole abdomen. In either case, pain typically starts as a generalized abdominal pain (with involvement of poorly localizing visceral innervation visceral peritoneal layer), and may become localized later (with involvement of the somatic innervation of the parietal peritoneal layer). Peritonitis is an example of an acute abdomen. Other symptoms • Diffuse abdominal rigidity (abdominal guarding) is often present, especially in generalized peritonitis • Fever • Sinus tachycardia • Development of ileus paralyticus (i.e., intestinal paralysis), which also causes nausea, vomiting and bloating • Reduced or no passage of abdominal gas and bowel sound Complications • Sequestration of fluid and electrolytes, as revealed by decreased central venous pressure, may cause electrolyte disturbances, as well as significant hypovolemia, possibly leading to shock and acute kidney failure. • A peritoneal abscess may form (e.g., above or below the liver, or in the lesser omentum) • Sepsis may develop, so blood cultures should be obtained. • Complicated peritonitis typically involves multiple organs. Physical examination In order to clinically examine a patient with an acute abdomen, it is necessary to: • Inspection for injuries or hematomas, hernias, other abdominal wall defects or skin discoloration (pancreatitis). The stomach participates in the act of breathing • Auscultation should always be performed prior to manual examination in order to avoid provoking intestinal noises. Intestinal sounds should be auscultated in 4 sections. Are there intestinal noises present? What grade are they? If no noises are heard, this could indicate a paralytic ileus. • Palpation to detect muscle rigidity, muscle guarding, peritonism (rebound tenderness), tenderness, and ascites. • Percussion helps in the detection of ascites, and abdominal fluid. • Digital rectal examination for conditions such as palpable tumors, an empty bowel (caused by an obstacle such as ileus or tumor) and blood. Physical examination • • • • • • • • • Abdominal signs • Cullen • Grey Turner • Kehr • Murphy • Romberg-Howship • Blumberg • Markle (heel jar) • Rovsing Other symptoms • Diffuse abdominal rigidity (abdominal guarding) is often present, especially in generalized peritonitis • Fever • Sinus tachycardia • Development of ileus paralyticus (i.e., intestinal paralysis), which also causes nausea, vomiting and bloating • Reduced or no passage of abdominal gas and bowel sound Key symptoms of acute abdomen 1. Abdominal pain The main manifestations of peritonitis are acute abdominal pain, abdominal tenderness, abdominal guarding, rigidity, which are exacerbated by moving the peritoneum, e.g., coughing (forced cough may be used as a test), flexing one's hips, or eliciting the Blumberg sign (meaning that pressing a hand on the abdomen elicits less pain than releasing the hand abruptly, which will aggravate the pain, as the peritoneum snaps back into place). Rigidity is highly specific for diagnosing peritonitis (specificity: 76–100%). The presence of these signs in a person is sometimes referred to as peritonism. The localization of these manifestations depends on whether peritonitis is localized (e.g., appendicitis or diverticulitis before perforation), or generalized to the whole abdomen. In either case, pain typically starts as a generalized abdominal pain (with involvement of poorly localizing visceral innervation visceral peritoneal layer), and may become localized later (with involvement of the somatic innervation of the parietal peritoneal layer). Peritonitis is an example of an acute treatment of acute abdomen Treatment tactics:Peritonitis is an absolute indication for emergency surgery. 1. Preoperative preparation: 1) antibiotic prophylaxis 60 minutes before the incision intravenously: 1.5 g of cefuroxime,· or 1.2 g of amoxicillin/clavulanate,· or 1.5 g of ampicillin/sulbactam;· or cephalosporins (in the above dosage) + 500mg metronidazole or 300 mg clindamycin - at high risk of contamination by anaerobic bacteria;· or 1 g of vancomycin - if you are allergic to beta-lactams or have a high risk of infection of the wound; 2) correction of dysfunctions caused by concomitant pathology; 3) nasogastric probe into the stomach to evacuate the contents of the stomach; 4) catheterization of the bladder; 5) hygienic preparation of the surgical intervention area. Treatment goals: 1.elimination of the source of peritonitis; 2.evacuation of pathological exudate, sanitation and drainage of the abdominal cavity; 3.source control (in case of abdominal sepsis), damage control (in case of injury); 4.elimination of disorders and restoration of the function of vital organs and systems. Surgical intervention With peritonitis without sepsis, it can be performed by a traditional and laparoscopic method and provides for radical elimination of the source. Anesthetic support: general anesthesia. • drainage of the abdominal cavity with rational placement of drains in the supposed places of exudate accumulation (with widespread peritonitis - in the subdiaphragmati c, subhepatic areas, left lateral canal, pelvis); • Options for completing the operation adequate surgical intervention with complete elimination of the source can be completed by rational drainage and suturing of the abdominal cavity. At the appearance of the first signs of progression of peritonitis or intra– abdominal complications requiring surgical correction - relaparotomy "on demand" Physical examination • • • • • Peritoneal signs • Guarding (voluntary-involuntary-rigidity) • Rebound • Heel jar/heel tap • Obturator test (pain in medial thigh with rotation) • • Iliopsoas test (passive extension/active flexion) • • Rovsing sign • • Pain out of proportion to exam