Biomedical Applications of Polymeric Microneedles for Transdermal Therapeutic Delivery and Diagnosis: Current Status and Future Perspectives
реклама
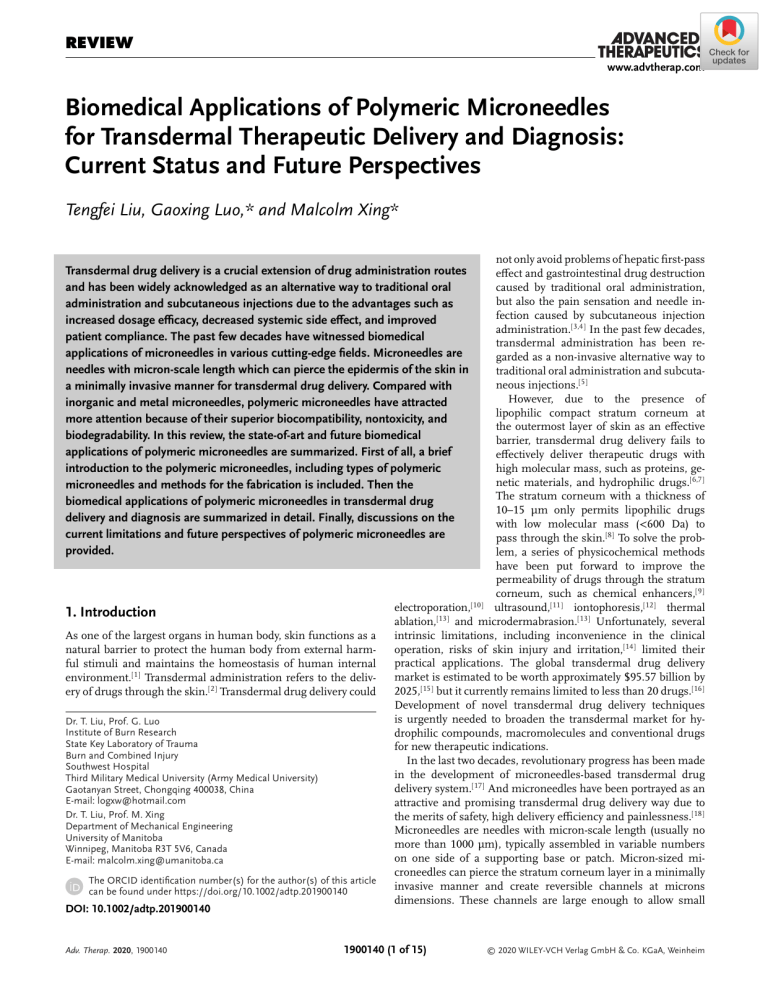
REVIEW www.advtherap.com Biomedical Applications of Polymeric Microneedles for Transdermal Therapeutic Delivery and Diagnosis: Current Status and Future Perspectives Tengfei Liu, Gaoxing Luo,* and Malcolm Xing* not only avoid problems of hepatic first-pass effect and gastrointestinal drug destruction caused by traditional oral administration, but also the pain sensation and needle infection caused by subcutaneous injection administration.[3,4] In the past few decades, transdermal administration has been regarded as a non-invasive alternative way to traditional oral administration and subcutaneous injections.[5] However, due to the presence of lipophilic compact stratum corneum at the outermost layer of skin as an effective barrier, transdermal drug delivery fails to effectively deliver therapeutic drugs with high molecular mass, such as proteins, genetic materials, and hydrophilic drugs.[6,7] The stratum corneum with a thickness of 10–15 µm only permits lipophilic drugs with low molecular mass (<600 Da) to pass through the skin.[8] To solve the problem, a series of physicochemical methods have been put forward to improve the permeability of drugs through the stratum corneum, such as chemical enhancers,[9] [10] electroporation, ultrasound,[11] iontophoresis,[12] thermal [13] and microdermabrasion.[13] Unfortunately, several ablation, intrinsic limitations, including inconvenience in the clinical operation, risks of skin injury and irritation,[14] limited their practical applications. The global transdermal drug delivery market is estimated to be worth approximately $95.57 billion by 2025,[15] but it currently remains limited to less than 20 drugs.[16] Development of novel transdermal drug delivery techniques is urgently needed to broaden the transdermal market for hydrophilic compounds, macromolecules and conventional drugs for new therapeutic indications. In the last two decades, revolutionary progress has been made in the development of microneedles-based transdermal drug delivery system.[17] And microneedles have been portrayed as an attractive and promising transdermal drug delivery way due to the merits of safety, high delivery efficiency and painlessness.[18] Microneedles are needles with micron-scale length (usually no more than 1000 µm), typically assembled in variable numbers on one side of a supporting base or patch. Micron-sized microneedles can pierce the stratum corneum layer in a minimally invasive manner and create reversible channels at microns dimensions. These channels are large enough to allow small Transdermal drug delivery is a crucial extension of drug administration routes and has been widely acknowledged as an alternative way to traditional oral administration and subcutaneous injections due to the advantages such as increased dosage efficacy, decreased systemic side effect, and improved patient compliance. The past few decades have witnessed biomedical applications of microneedles in various cutting-edge fields. Microneedles are needles with micron-scale length which can pierce the epidermis of the skin in a minimally invasive manner for transdermal drug delivery. Compared with inorganic and metal microneedles, polymeric microneedles have attracted more attention because of their superior biocompatibility, nontoxicity, and biodegradability. In this review, the state-of-art and future biomedical applications of polymeric microneedles are summarized. First of all, a brief introduction to the polymeric microneedles, including types of polymeric microneedles and methods for the fabrication is included. Then the biomedical applications of polymeric microneedles in transdermal drug delivery and diagnosis are summarized in detail. Finally, discussions on the current limitations and future perspectives of polymeric microneedles are provided. 1. Introduction As one of the largest organs in human body, skin functions as a natural barrier to protect the human body from external harmful stimuli and maintains the homeostasis of human internal environment.[1] Transdermal administration refers to the delivery of drugs through the skin.[2] Transdermal drug delivery could Dr. T. Liu, Prof. G. Luo Institute of Burn Research State Key Laboratory of Trauma Burn and Combined Injury Southwest Hospital Third Military Medical University (Army Medical University) Gaotanyan Street, Chongqing 400038, China E-mail: logxw@hotmail.com Dr. T. Liu, Prof. M. Xing Department of Mechanical Engineering University of Manitoba Winnipeg, Manitoba R3T 5V6, Canada E-mail: malcolm.xing@umanitoba.ca The ORCID identification number(s) for the author(s) of this article can be found under https://doi.org/10.1002/adtp.201900140 DOI: 10.1002/adtp.201900140 Adv. Therap. 2020, 1900140 1900140 (1 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com molecular drugs, macromolecules (peptide, protein, vaccine, nucleic acid), nanoparticles, and interstitial fluid to pass through the stratum corneum for local or systemic treatments/diagnosis.[19] Besides, the length of microneedles determine that the maximal insertion depth only reaches epidermis. Such insertion depth will not stimulate or damage nociceptive nerves and blood vessels in the dermis (1–2 mm in thickness), thus causing no pain or potential skin injury.[20] Generally, the length of the microneedle is between 100 and 1000 µm, and microneedle tips range from 1 to 10 µm.[20] As the force required to insert microneedles into the skin increased with insertion depth,[21] the mechanical strength, insertion depth, and drug release profile of microneedles could be adjusted by modulating and altering microneedle geometry and composition according to the target drugs and applications. Modulation of microneedle geometry could change the mechanical strength and insertion depth. Alteration of microneedle composition with dissolving, degradable, or non-dissolvable materials could adjust drug release profiles to realize rapid, slow-sustained, or stimuli-responsive drug release.[22] The concept of microneedles was first introduced in the 1970s by Gerstel and Place.[23] But due to the lack of techniques to fabricate such small needles, transdermal drug delivery efficacy of microneedles was not reported until 1998 when Prausnitz et al. fabricated the silicon microneedles for transdermal delivery of calcein. They demonstrated that the drug permeability of skin was enhanced by fourfold due to the conduits formed by microneedles.[24] This report was a landmark innovation which opens the era of microneedle-based transdermal drug delivery. Since then, a variety of materials have been used to fabricate microneedles for transdermal delivery of drugs, genetic materials, vaccine, macromolecules, nanoparticles, and even cells. Despite that no microneedle-based product is currently available in the clinic, 69 clinical trials regarding microneedle-based transdermal drug delivery have been completed according to the data obtained from the clinical trial website.[15] According to the composition of materials, microneedles can be classified into inorganic microneedle (such as silicon and glass microneedles), metal microneedles (such as stainless steel and titanium microneedles) and polymeric microneedles (such as hyaluronic acid, chitosan, polyacrylic acid, and polymethyl methacrylate microneedles).[25] Inorganic microneedles are brittle and prone to be fractured in the skin. Although metal microneedles could pierce the skin and increase the drug permeability, they have limited drug loading capacity, risks of skin rupture, and expensive and complex fabrication process. These drawbacks limit the biomedical application of these two types of microneedles.[26] Polymeric microneedles are the current research hotspot in transdermal drug delivery due to unique advantages such as easy and inexpensive fabrication process, excellent biocompatibility, and high drug loading amount.[27–29] More importantly, polymeric microneedles could be fabricated by a plethora of polymeric materials with different degradation/swelling profiles, and biological/physical stimuli-responsive properties, which increase the tunability of designing microneedles with controllable drug release profile for versatile biomedical applications. In this review, we attempt to discuss recent advances in the development of polymer microneedles for transdermal drug Adv. Therap. 2020, 1900140 Tengfei Liu received his bachelor’s degree and master’s degree from the Army (Third Military) Medical University, Chongqing, China. He is currently pursuing his Ph.D. degree under the joint supervision of Prof. Gaoxing Luo and Prof. Malcolm Xing. His research focuses on the development of stimuli-responsive biomaterials for wound repair and infection control. Gaoxing Luo received postdoctoral training in Yale University in the United States. He is currently working as the director, professor, and surgeon in the Institute of Burn Research, Southwest Hospital, Army (Third Military) Medical University, China. He also serves as the vice chairman of the Chinese Burn Association. His research interests include the application of stem cells for tissue engineering and the development of interdisciplinary strategies for wound repair and regeneration. Malcolm Xing is a professor of University of Manitoba, Canada. His research focuses on smart biomaterials for tissue engineering, nanomedicine, wearable biosensors, implantable biorobot and 3D/4D bioprinting. delivery and biological fluid monitoring and diagnosis. It will be reviewed in detail from the types of polymeric microneedles to methods for fabricating polymeric microneedles. Then we focus on the biomedical applications of polymeric microneedles in transdermal drug delivery and diagnosis and future perspectives of this field will be discussed. 2. Types of Polymeric Microneedles A variety of polymers with different characteristics have been utilized to fabricate polymeric microneedles, as shown in Table 1. According to the in vivo performance of microneedles, polymeric 1900140 (2 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Table 1. Representative polymers used for fabricating microneedles (references are listed in the corresponding sections). Microneedle type Polymers Dissolving microneedles Hyaluronic acid (HA), sodium alginate, dextran, gelatin, polyvinylpyrrolidone (PVP), hydroxypropyl cellulose (HPC), carboxymethylcellulose (CMC), hydroxypropyl methylcellulose (HPMC), poly-l-glutamic acid (𝛾-PGA), sodium chondroitin sulfate, amylopectin Degradable microneedles Polycaprolactone (PCL), polylactic acid (PLA), polyglycolic acid (PGA), poly(lactic-co-glycolic acid) (PLGA), polycarbonate (PC), chitosan Non-dissolvable microneedles polystyrene (PS), polymethyl methacrylate (PMMA), polyvinyl alcohol (PVA), poly(methyl vinyl ether-co-maleic acid) (PMVE-co-MA), acrylate modified HA (m-HA), poly(2-hydroxyethyl methacrylate) (PHEMA) microneedles can be classified into dissolvable microneedles, non-dissolvable microneedles and hybrid microneedles.[30] Dissolvable microneedles can be further divided into dissolving microneedles and degradable microneedles.[31] The polymeric matrix could incorporate drugs and protect drugs from physical or biological disruption. After insertion into the skin, microneedles would dissolve, swell, or degrade and then release the loaded drugs.[32] The materials for fabricating dissolvable microneedles mainly include hyaluronic acid (HA), sodium alginate, polyvinylpyrrolidone (PVP), hydroxypropyl cellulose (HPC), carboxymethylcellulose (CMC), dextran, hydroxypropyl methylcellulose (HPMC), poly-l-glutamic acid (𝛾-PGA), sodium chondroitin sulfate, gelatin, and amylopectin.[33–35] Drug-loaded microneedles fabricated by water-soluble polymer matrix generally dissolve rapidly and completely after being inserted into the skin, producing no biohazardous medical waste.[36] The rapid dissolution of microneedles results in the rapid release of loaded drugs. This indicated that dissolving microneedles can be utilized to realize instant transdermal drug delivery.[37] For example, Mönkäre et al. reported that monoclonal IgG-loaded dissolvable HA microneedles were able to penetrate the epidermis of excised human skin and the majority of inserted needle tips were dissolved after being inserted into skin for 10 min.[38] Kim et al. fabricated dissolvable microneedles of which the needle tips and base were made of HPMC and CMC, respectively.[39] After being inserted into the skin, HPMC tips which encapsulated the drug (donepezil hydrochloride) dissolved quickly within 15 min. A plethora of materials have been used for the fabrication of degradable microneedles, including polycaprolactone (PCL), polylactic acid (PLA), polyglycolic acid (PGA), poly(lactic-co-glycolic acid) (PLGA), polycarbonate (PC), and chitosan.[40–44] For drug-loaded microneedles fabricated by degradable polymer matrix, drug release profiles are closely related to the degradation behaviors of substrate materials.[45] And the loaded drugs are slowly released with the degradation of polymers. Fabricating dissolvable composite microneedles by combining soluble polymeric materials with degradable polymeric materials is a novel way to realize rapid separation of support from tips and controlled drug release.[46,47] For example, Chen et al. prepared a dissolvable composite microneedle of which the tip was made of PCL and the support was constituted of polyvinyl alcohol (PVA) and PVP.[27] When the microneedles were inserted into the skin, the support dissolved and separated from tips, leaving the PCL tips containing doxorubicin and lanthanum hexaboride in the skin to achieve slow-sustained drug release. Adv. Therap. 2020, 1900140 Non-dissolvable microneedles are generally utilized for skin pretreatment. Non-dissolvable microneedles could pierce the stratum corneum of skin and form micron-sized channels for the drug in a patch to directly pass through the stratum corneum or could achieve transdermal drug delivery by coating the drug solution directly on the microneedle surface.[48] The constitutional materials of conventional non-dissolvable microneedles mainly include polystyrene (PS) and polymethyl methacrylate (PMMA).[49,50] With the rapid development in designing and fabricating microneedles, a new type of non-dissolvable microneedle, namely hydrogel microneedle, has become a research hotspot in polymeric microneedles due to its unique capability of swelling. Hydrogel microneedles are fabricated through the physical or chemical cross-linking of polymeric matrix, which could confer sufficient mechanical strength to the microneedle to pierce the stratum corneum of skin.[51] Compared with dissolvable microneedles, crosslinked hydrogel microneedles would swell but not dissolve when inserted into the skin. This property makes it possible for the extraction of interstitial fluid from the skin and release of pre-loaded drugs during the swelling process.[52] For interstitial fluid extraction, hydrogel microneedles swelled and subsequently the interstitial fluid containing biomarkers would be imbibed into the microneedles. For drug delivery, drug-loaded hydrogel microneedles swelled and the preloaded drugs subsequently diffused out the microneedles. Furthermore, no substrate would remain in the skin when microneedles are pulled out of the skin. This suggests that hydrogel microneedles have proper biosafety and are suitable for repeated use over a long period of time.[53] Adjusting the swelling ability of polymers by controlling the cross-linking density could improve the transdermal drug delivery efficiency and drug release behavior.[54,55] The substrate materials for the preparation of hydrogel microneedles mainly include PVA, poly(methyl vinyl ether-co-maleic acid) (PMVE-co-MA), acrylate modified HA (mHA), and poly(2-hydroxyethyl methacrylate) (PHEMA).[56–58] It is worth noting that the cross-linking process of polymers usually involves high temperature or UV exposure,[59] it is necessary to protect the loaded protein drugs from disruption throughout the fabrication process by loading drugs into the base postmolding instead of the microneedle tip during cross-linking process.[60] Furthermore, it should be noted that swellable microneedles require fine tuning of the cross-linking density so as to possess sufficient mechanical strength in the dry state to pierce the stratum corneum. Besides, they need to maintain good mechanical strength in the hydrated state so as to be completely removed from skin. 1900140 (3 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 1. Schematic illustration of polymeric microneedle fabrication by A) micromolding. Adapted with permission.[30] Copyright 2016, Elsevier Ltd. B) 3D printing. Adapted with permission.[94] Copyright 2018, Royal Society of Chemistry. C) Drawing lithography. Adapted with permission.[78] Copyright 2012, Elsevier Ltd. (D) Droplet-born air blowing methods. Adapted with permission.[75] Copyright 2013, Elsevier Ltd. Hybrid microneedles generally use two or more materials with completely different properties to achieve special functions through the optimization of microneedle structure.[61,62] It is worth noting that hybrid microneedles do not necessarily have to be all polymeric. They could be fabricated through the hybridization of polymers, metals or inorganic substance. For example, Lee et al. reported the fabrication of hybrid microneedles with maltose (MT) and metal electrodes through drawing lithography technique.[63] Compared with pure metal microneedles, the tip of maltose needle has higher gene loading capacity. By combining with metal electrodes which can generate pulsed electric fields, this hybrid microneedle significantly improves the gene transfection efficiency. Prausnitz et al. reported the preparation of hybrid microneedles made of PVA/PVP and stainless steel to achieve rapid separation of the tip from the support and release the drug by using water soluble property of the tip polymer, which provides a rapid, convenient, and safe way of transdermal drug delivery.[64] Cao et al. reported the fabrication of hybrid PVA/MT microneedles to deliver anti-inflammatory drugs.[65] The mechanical strength of PVA microneedles were significantly improved after adding MT. Once inserted into the skin, MT dissolved completely, thus generating micropores for the release of drugs from polymeric matrix. For hybrid microneedles, it is necessary to fine tune the composition ratio and structural distribution of substitute polymers so as to optimize the drug release profile and mechanical toughness. Adv. Therap. 2020, 1900140 3. Methods for the Fabrication of Polymeric Microneedles With the rapid development of science and technology, more and more versatile microneedle fabrication techniques have emerged in the past few decades. Figure 1 shows several commonly used fabrication processes of microneedles. Micromolding is the most commonly used method to fabricate polymeric microneedles because of excellent reproducibility, cost-efficiency, and convenience for scalable production.[66] Micromolding utilizes laser etching, ion etching, and other methods to directly or indirectly fabricate microneedle molds with desired size and morphology. Then the desired polymers are added to the mold to fabricate corresponding polymeric microneedles.[67] According to the different processing methods of polymers in the microneedle mold, the micromolding method can be divided into casting method, hot embossing method, injection molding and investment molding, and so forth.[30] In general, casting method casts the drugloaded polymer solution into the microneedle mold, and promotes the polymer solution into the holes of microneedle mold by centrifugation, vacuum or ultrasound to eliminate bubbles, and then dry the mold to obtain the desired microneedle.[26,68,69] Due to the advantages of low processing temperature, convenient fabrication process and little impact on drug activity, casting method is currently the most commonly used method to prepare dissolvable polymer microneedles.[70,71] Hot embossing 1900140 (4 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com method, injection molding and investment molding are usually used to prepare degradable and insoluble microneedles, but the processing temperature is relatively high in general, which might easily affect the drug activity.[72,73] Although micromolding method does have some advantages, some limitations such as time-consuming complex fabrication steps, involvement of heat or UV irradiation in the fabrication process might reduce the activity of sensitive drugs.[74] Different from micromolding method, some novel methods, such as drawing lithography, droplet-born air blowing, electro-drawing and 3D printing, do not require the use of a mold and can achieve rapid (usually within 10 min) microneedle preparation.[42,75–77] The drawing lithography method directly extends the 2D thermosetting polymer materials to acquire the 3D polymeric microneedles.[76] Compared with conventional micromolding, drawing lithography method not only can fabricate microneedles with high aspect ratio, but also eliminates the need for molds and UV light irradiation, thereby avoiding the use of toxic photoinitiators.[78] However, since the formation of microneedles strongly depends on the dynamic interaction between the fluid and frame, many factors including the viscous property of the thermosetting polymer fluid, the patterns of the contacting pillars, and the drawing rate of the frame would affect the final shape of the microneedles. Therefore, drawing lithography method exhibits much worse reproducibility than micromolding.[42] Besides, it requires high temperature for stretching and curing of thermosetting polymers, which limits the delivery of heat-sensitive drugs.[79] On the contrary, the fabrication processes of droplet-born air blowing method, electro-drawing method, and 3D printing method (inkjet printing, photopolymerization-based technique) are relatively mild. The droplet-born air blowing method shapes polymer droplets into dissolvable polymeric microneedles by air flow,[75] and electro-drawing method uses electrofluid actuation which is not contacted at room temperature to fabricate degradable polymeric microneedles.[42] However, conventional microneedle fabrication techniques mentioned above cannot fabricate microneedles on curved surfaces. As traditional microneedles are fabricated on the flat substrate surface, it is difficult to completely insert into uneven or curved skin surface, which results in the decreased penetration efficiency and drug delivery amount. Due to the versatility and tunability to rapidly fabricate physical models of any geometrical shape up to micron scale with the computer-aided design and computer-aided manufacturing,[80] 3D printing technology has been utilized for the personalized fabrication of polymeric microneedles with desired shapes and architectures in the last decade.[81,82] 3D printing is a rapid prototyping technology based on layer-by-layer printing and layer-by-layer superposition, which has the advantages of high accuracy, good reproducibility, and one-step fabrication and can meet personalized needs.[83,84] The currently commonly utilized manufacturing technologies of 3D printing for the fabrication of polymeric microneedles mainly include inkjet printing, photopolymerization-based technique, and fused deposition modelling (FDM).[85] Inkjet printing could achieve controllable and selective deposition of drug droplets onto microneedle surface by numerous thermal or piezoelectric-driven printing heads.[86] Currently, such technique has been main utilized to coat pre-fabricated microneedles with drugs for the personalized and combined drug loading.[87,88] Adv. Therap. 2020, 1900140 Photopolymerization-based technique refers to the fabrication of 3D models by selectively polymerization of photo-sensitive polymers under the laser/light irradiation. Such technique could fabricate polymeric microneedles by consistent layer-by-layer polymerization of UV-sensitive polymers through the photopolymerization curing process.[89] Stereolithography (SLA), digital light processing (DLP), and two-photon polymerization (2PP) are the commonly used photopolymerization-based techniques to fabricate polymeric microneedles.[90–92] The printing speed of DLP is generally faster than SLA as the whole layer is fabricated simultaneously. While 2PP is suitable for the fabrication of elaborate, complex structures in the microscale and nanoscale. Lim et al. used DLP to fabricate a novel microneedle on personalized curved surfaces to realize complete insertion of microneedle into the contoured human skin.[81] The adoption of SLA, DLP, and 2PP technologies for the fabrication of polymeric microneedles is an attractive concept because of the versatility in geometric complexity and high needle resolution provided by these technologies.[93,94] However, some photoinitiators used in the photopolymerization process are toxic and have certain health concerns in transdermal drug delivery.[77] FDM, a subset of extrusion printing, is a versatile, cost-effective 3D printing technique on the basis of the melt-extrusion process and could print biodegradable materials. However, there are some major disadvantages of such technology, such as poor resolution, and limited variety of substitute materials.[85,95] Currently its applications in microneedle fabrication are still limited in literature. Nevertheless, FDM is still an appealing method as the fabrication process eliminates the use of solvents.[96] Besides, there are currently some reports on the combination of FDM with post-fabrication chemical etching step to fabricate biodegradable microneedles with high resolution.[94] The skin penetration ability of polymeric microneedles is closely related to the geometry characteristics including shape, aspect ratio, and tip diameter.[20,31,71] Up to now, the vast majority of microneedles are fabricated typically in cone or pyramid shapes. Pyramidal shaped microneedles generally possessed better mechanical strength than the conical shaped ones.[97] As for microneedles with same needle shapes, the mechanical strength was improved by decreasing the aspect ratio or increasing the base width.[98] But it is worth noting that excessively increasing the base width to reduce the aspect ratio will decrease the skin insertion efficiency of microneedles.[99] As for tip diameter, microneedles with sharper tips generally could insert into the skin more easily than the blunt one. For example, Chen et al. reported that chitosan microneedles with a tip diameter of 10 µm could penetrate twice as deep as those with a tip diameter of 20 µm.[19] In general, pyramidal shaped polymeric microneedles with smaller tip diameter and aspect ratio possess better penetration efficiency. 4. Biomedical Applications of Polymeric Microneedles for Transdermal Drug Delivery Polymeric microneedles in general could achieve percutaneous delivery of peptides, proteins, vaccines, and small molecule drugs. Based on the difference in drug release behavior, polymeric microneedles can be classified into rapid drug-releasing 1900140 (5 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 2. A) Brightfield (a) and fluorescence micrographs of exenatide loaded HA microneedles before (b) and after (c) skin insertion for 2 min. Fluorescence (d) and merged brightfield and fluorescence images of porcine skin puncture sites (white arrows) (e). The green fluorescence represents exenatide. Adapted with permission.[100] Copyright 2014, Springer. B) Images of traditional microneedles and rapidly separating microneedles before and after insertion into pig skin for different time points. Adapted with permission.[101] Copyright 2016, Elsevier Ltd. type, slow-sustained drug-releasing type and stimuli-responsive drug-releasing type. 4.1. Rapid Drug-Releasing Polymeric Microneedles The rapid drug-releasing polymeric microneedles generally encapsulate the drugs in water-soluble polymeric tips. There are various substrate materials for the preparation of microneedle support, including dissolving polymers, degradable polymers, and metal matrices. Tuning the composition and architecture of microneedle tip and support could achieve in situ rapid release of loaded drugs, which could significantly increase the instantaneous drug concentration. Wang et al. reported the preparation of hyaluronic acid microneedles which contained exenatide drug at the needle tip using a casting method (as shown in Figure 2A).[100] In vitro drug release results showed that the microneedles released approximately 80% of loaded drugs after being inserted into the skin for 30 s, and almost all of the encapsulated drugs were released in 2 min. Furthermore, in vivo animal experimental results showed that the therapeutic effect of this microneedle for type II diabetes was comparable to that of conventional subcutaneous injection of insulin, with a relative bioavailability of up to 97%. Guo et al. used Rhodamine B as a model drug to prepare dissolvable PVA/sucrose/PLA composite microneedles loaded with Rhodamine B at the needle tip.[101] Adv. Therap. 2020, 1900140 The tip of microneedle was PVA/sucrose which could easily dissolve in water, and the microneedle support was biodegradable PLA. More than 90% of the loaded drugs could be released after being inserted into the skin for 30 s, indicating a fast and highly efficient transdermal drug delivery manner (as shown in Figure 2B). 4.2. Slow-Sustained Drug-Releasing Polymeric Microneedles Long-term slow-sustained drug release can maintain a stable blood concentration, prolong the duration of drugs, and reduce toxic side effects. Slow-sustained drug-releasing polymeric microneedles usually use hydrogel microneedles to control the drug release rate by adjusting the cross-linking density at the physical or chemical cross-linking point. Jin et al. reported the fabrication of insulin-loaded PVA phase-change microneedles which was prepared by using a freeze-thaw physical cross-linking method.[29] Animal experimental results indicated that the insulin content delivered percutaneously by the insulin-loaded microneedle patch (dose: 2.0 IU·Kg−1 ) reached a peak at about 1 h, followed by a slow and sustained release for 3 h. The blood insulin of pigs attached with two insulin-loaded microneedles (dose: 2.0 IU·Kg−1 ) was comparable to those treated with conventional insulin pen (dose: 0.4 IU·kg−1 ), which indicated that the relative bioavailability of the insulin microneedle was as high 1900140 (6 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 3. A) Schematic illustrations of transdermal delivery of macromolecules using chitosan microneedle patches. Adapted with permission.[99] Copyright 2012, American Chemical Society. B) Schematic illustrations of sustained transdermal delivery of antigen using a microneedle delivery system, composed of embeddable chitosan microneedles and a PLA supporting array. Adapted with permission.[105] Copyright 2013, Elsevier Ltd. as 20%. Due to the absence of chemical crosslinkers during the microneedle fabrication process, bioactive drugs such as proteins and peptides could be easily loaded on the microneedles in a mild manner. Donnelly et al. reported the fabrication of hydrogel microneedles using PMVE-co-MA copolymer, polyethylene glycol (PEG), and sodium bicarbonate as raw materials to achieve esterification cross-linking at 80 °C.[54] Besides, the integration of drug-loaded patches into the hydrogel microneedles allows the construction of a chemically cross-linked hydrogel microneedle system with slow-sustained drug release for 24 h. Due to the presence of drug-loaded patch, the drug loading capacity of the hydrogel microneedles could be increased up to several milligrams. Meanwhile, the hydrogel microneedles could also achieve better transdermal drug delivery when combined with iontophoresis. In addition, slow-sustained drug releasing polymeric microneedles could also be fabricated using degradable polymeric matrix which degraded slowly and gradually released drugs in vivo. There are numerous intricate and complicated factors that can affect the in vivo polymer degradation behavior including both internal factors, such as the composition, chain structure, aggregation state of the polymer, and external factors, such as temperature, oxygen, water, and light. Chen et al. reported the preparation of bovine serum albumin (BSA)-loaded chitosan microneedles by casting method using 80% deacetylated chitosan as raw material (as shown in Figure 3A).[99] It was shown by circular dichroism spectroscopy that the conformation of the protein in the microneedle was almost unaffected. On the one hand, as chitosan dissolved easily under weakly acidic aqueous conditions, no organic solvents or harsh conditions of heat was needed in the mixture of bioactive molecules with chitosan. On the other hand, chitosan has excellent biocompatibility, degradability and nontoxicity, which would not affect the conformation and activity of bioactive molecules such as proteins.[102] The in vitro drug release test results demonstrated that the microneedle could sustained and cumulatively release 95% drugs within 8 days. Since the skin contains a large number of immunocompetent cells (Langerhans cells, dendritic cells, etc.) which can trigger the Adv. Therap. 2020, 1900140 adaptive immune response, compared with the traditional intramuscular injection of vaccine, transcutaneous immunization requires less antigen to produce a stronger immune effect.[103,104] The transcutaneous immunization via microneedles was further studied by Chen et al.,[105] who prepared chitosan/PVP/PLA composite dissolvable microneedles using ovalbumin (OVA) as a model antigen, as shown in Figure 3B. OVA is the main protein found in chicken egg white, which has been widely used as a model antigen in immunological studies due to its good immunogenicity. The microneedle tip was chitosan loaded with OVA model antigen, and the support of microneedle was PLA. The contact surface between PLA and chitosan was coated with PVP. When chitosan/PVP/PLA composite microneedles were inserted into the skin for 5 min, the skin interstitial fluid would dissolve the PVP coating, resulting in the separation of the PLA support from the chitosan needle tip and the retention of the OVA-loaded chitosan needle tip in the skin. The OVA antigen was continuously released as the chitosan tip slowly degraded in the skin. On day 7 post microneedle insertion, a strong OVA-specific antibody response could be detected and lasted for 6 weeks, indicating excellent long-lasting sustained release behavior of the microneedle and great potential for sustained transcutaneous immunization by microneedles. 4.3. Stimuli-Responsive Drug-Releasing Polymeric Microneedles Constructing stimuli-responsive gene/drug delivery system is one of the hotspots in gene/drug delivery field.[106–108] Stimuli from physiological condition (pH value, glucose concentration, enzyme activity, etc.) or external environment (sound, light, electric current, magnetic field, temperature, strain, etc.) have been used as the trigger for the release of drugs in the microneedle. Polymeric microneedles with stimulus-responsive properties are expected to achieve on-demand administration and better therapeutic effects. It is worth noting that several important issues regarding the safety, pharmacokinetics, therapeutic efficacy, costs of manufacture, storage and transportation 1900140 (7 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 4. A) Schematic illustration of the design of the PVP microneedle arrays containing pH-responsive PLGA HMs and their mechanism for codelivery of two different model drugs Alexa 488 and Cy5 in sequence. Adapted with permission.[68] Copyright 2012, Elsevier Ltd. B) Schematic of the glucose responsive system based on a microneedle-array patch. The patch integrated with pancreatic 𝛽-cells but without glucose signal amplifiers (a). The patch integrated with pancreatic 𝛽-cells and glucose signal amplifiers (b). Adapted with permission.[109] Copyright 2016, Wiley-VCH. should be thoroughly evaluated prior to clinical translation of stimulus-responsive microneedles. 4.3.1. Stimuli-Responsive Drug Release Triggered by Internal Physiological Environment Stimuli-responsive drug release behavior of microneedles could be triggered by changes in the human body’s intrinsic physiological signals, such as pH value, glucose concentration and enzyme activity, so as to release the entrapped drugs, realize on-demand administration and even regulate the speed of administration.[68,108,109] Stimuli-responsive drug-releasing microneedles would no doubt provide a new approach for personalized treatment in the future. Taking advantage of the acidic nature of the human skin epidermis, Sung et al. prepared a PVP microneedle with sequential drug release property in response to pH stimulation, as shown in Figure 4A.[68] In the first step, they prepared polylactic acidglycolic acid copolymer (PLGA) microspheres which encapsulated the model drug 2 (Cy5) and the foaming agent sodium bicarbonate (NaHCO3 ). Then, using PVP as the raw material, PVP microneedle loaded with free model drug 1 (Alexa 488) and drug-loaded PLGA microspheres was prepared by micromolding method. When PVP microneedles were inserted into the skin for 5 min, more than 50% of free model drug 1 was released rapidly. Due to the acidic nature of the skin epidermis, H+ permeated into PLGA microspheres, dissolved NaHCO3 and produced CO2 . CO2 could generate micropores on the microsphere surface and thereby promote the release of model drug 2, allowing more than 50% of model drug 2 to be released within 15 min. Such strategy using acidic microenvironment of the skin epidermis to regulate the release order of a variety of drugs has great potential in clinical Adv. Therap. 2020, 1900140 medical applications. For example, cardiovascular agonists are usually administered 15–20 min before the therapeutic agent.[110] Diabetes is a metabolic disease characterized by hyperglycemia. In the 21st century, diabetes has become one of the most serious public health problems in the world. To solve this public health problem, Gu et al. prepared a smart microneedle patch which could secrete insulin in response to glucose stimulation, as shown in Figure 4B. They innovatively designed a glucose signal amplifier (GSA) which is a hypoxia responsive hyaluronic acid vesicle containing glucose oxidase, 𝛼-linear amylase, and glucoamylase.[109] The control group was the GSA free microneedle patch consisting of cross-linked hyaluronic acid (HA) microneedles loaded with a microgel-containing pancreatic 𝛽 cells. When the microneedle was inserted into the skin, as the glucose content in the body increased, glucose would enter into the microneedle by diffusion, which in turn contacted with the pancreatic 𝛽 cells in the microgel at the bottom of the microneedle and then stimulated pancreatic 𝛽 cells to secrete insulin. However, due to the limited diffusion depth of glucose in the microneedle, the therapeutic effect was not quite obvious. In comparison, microneedle patches containing GSA and 𝛼-linear amylase at the tip of the needle exhibited highly efficient blood glucose regulation ability. With the increase of glucose content in the body, local hypoxia was generated under the action of glucose oxidase, which destroyed the amphipathic structure of GSA vesicles and promoted the release of encapsulated 𝛼-linear amylase, glucose oxidase and glucoamylase in GSA vesicles. Linear amylase could convert starch into disaccharides and trisaccharides, and then into glucose under the action of glucoamylase. The increase of local glucose content in the microneedle significantly enhanced the sensing ability of pancreatic 𝛽 cells and promoted rapid insulin secretion into the blood vessels and lymphatic capillary network, maintaining blood glucose at normal levels for up to 10 h. This design used a glucose amplifier to improve the stimulation sensitivity of pancreatic 𝛽 cells, exhibiting good 1900140 (8 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 5. A) Schematic illustrations of combination of chemotherapy and photothermal therapy using near-infrared light-activatable microneedles. Adapted with permission.[27] Copyright 2015, American Chemical Society. B) Schematic illustration of the tensile strain-triggered drug release. Adapted with permission.[111] Copyright 2015, American Chemical Society. blood glucose regulation efficiency. It is worth mentioning that in this microneedle system, the amount of glucose oxidase used in the microneedle is a key factor to trigger glucose-stimulated insulin secretion to regulate blood glucose concentration. If the content of glucose oxidase is too low, the hypoxic stimulation will lag behind, and pancreatic 𝛽 cells cannot secrete insulin in a timely and efficient manner to achieve the therapeutic effect. However, the human physiological environment is complex and variable. Even though drug release in response to physiological environmental stimuli can regulate the drug release behavior according to the magnitude of the stimulus signal, it has poor spatiotemporal controllability and is difficult to precisely control the amount of drugs administered.[111] 4.3.2. Stimuli-Responsive Drug Release Triggered by Changes in External Environment Stimuli-responsive drug release system triggered by changes in external environment conditions can generally be achieved by external stimulation signals such as light, temperature, stress, magnetic field, and ultrasound.[27,108,112] Such system is simple, convenient to operate, space-time controllable, and highly targeting. It can achieve administration or interruption at any time according to actual needs, providing great flexibility to patients. McCoy et al. reported the preparation of a UV lightresponsive drug-releasing polyhydroxyethyl methacrylate hydrogel microneedle.[59] The photo-responsive ibuprofen conjugate was immobilized in the microneedle matrix via non-covalent bonds, and the drug was trapped inside the microneedle without illumination. Upon UV illumination, the ibuprofen conjugate disintegrated and generated a water-soluble ibuprofen. Then ibuprofen diffused into the skin via the tissue fluid in the swollen microneedle to achieve a therapeutic effect. Ultraviolet light irradiation can control drug release and administer drugs on demand, but it has potential harm to the skin, thus limiting the practical application of this design. However, Adv. Therap. 2020, 1900140 other external stimulation factors such as near-infrared light and stress stretching have received more and more attention in recent years due to their safety and reliability. The penetration ability of near-infrared light into human body is strong, and it can penetrate deep subcutaneous tissue. When combined with photosensitizers or photothermal therapeutic agents, it could achieve locally targeted and highly effective treatment of tumors. Chen et al. prepared a near-infrared photostimulation-responsive drug releasing microneedle system containing doxorubicin (DOX) and lanthanum hexaboride (LaB6 ) nanomaterials by micromolding,[27] as shown in Figure 5A. The microneedle system used drug-loaded PCL as the tip and PVA/PVP as the support structure. When the microneedle was inserted into the skin for 5 min, the PVA/PVP support structure detached from the PCL needle tip, leaving the tip in the skin. Since PCL was hydrophobic, drugs could not be released. Upon near-infrared light irradiation, LaB6 nanomaterial underwent photothermal transformation, which increased the temperature of the targeted tissue for microneedle action and resulted in photoelimination. Meanwhile, PCL melted at 50 °C and then released the chemotherapeutic drug DOX, thus realizing the synergistic photothermal therapy and chemotherapy to kill the tumor. Lightactivated drug release can be precisely controlled and turned on or off as needed. At the same time, in vivo animal experimental results showed that when using laser irradiation for 3 times within 1 week, this collaborative treatment system can completely eradicate 4T1 breast tumors without tumor recurrence and significant weight loss, showing excellent therapeutic effect. Strain-responsive drug release, which does not require additional auxiliary equipment, is a simple way to construct wearable drug delivery system with on-demand release. Wearable drug delivery systems generally incorporate functional therapeutic carriers into flexible and stretchable supporting materials such as elastomers, hydrogels, and fabrics for noninvasive or minimally invasive delivery of pharmacological agents.[5] Gu et al. reported the preparation of microneedle-based wearable transdermal drug delivery system with stretch-triggered drug release property. They prepared the insulin-loaded PLGA 1900140 (9 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com nanoparticles, and then encapsulated the PLGA nanoparticles into sodium alginate microgel as the drug reservoir, as shown in Figure 5B.[111] The alginate microgel reservoir was then integrated with high-performance silicone elastomers (Dragon Skin 30) and hyaluronic acid microneedles into a wearable microneedle system with stress stimuli-responsive drug release. The microneedle system could act anywhere on the skin, no matter whether it is the flat skin, the bent knuckles, or elbows. When the microneedle attached place was stretched due to movement, the elastomer would be stretched, the surface area of the microgel increased and Poisson’s ratio changed, causing compression and promoting drug release to achieve therapeutic effects. Consequently, sustained drug release could be achieved by daily body motions of patients, and pulsatile drug release could be activated by intentional administration. 5. Biomedical Applications of Polymeric Microneedles for Diagnosis Apart from transdermal drug delivery, polymeric microneedles have also been utilized for the disease diagnosis and metabolic analysis due to the fact that they can extract the skin interstitial fluid (ISF) in a minimal invasive way than other techniques such Figure 6. A) Schematic representation of the rapid extraction of ISF by crosslinked MeHA-MN patches. Adapted with permission.[118] Copyright 2017, Wiley-VCH. B) Schematic illustration of the tensile strain-triggered drug release. Adapted with permission.[119] Copyright 2018, American Association for the Advancement of Science. Adv. Therap. 2020, 1900140 1900140 (10 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com as suction-blister technique and micropipettes insert.[44,113,114] ISF is generated from blood transcapillary filtration. Therefore, the constituent in the ISF is quiet similar to the plasma, which means that the ingredient changes in the ISF could represent changes in the human body.[115,116] Since hydrogel microneedles have the capability of swelling in the skin, they have been widely designed to extract ISF for monitoring and diagnosis. The extracted ISF samples could be separated from microneedles by centrifugation.[117] For example, Chang et al. reported the fabrication of a swellable microneedle made of methacrylated hyaluronic acid (MeHA), as shown in Figure 6A.[118] Due to the high water affinity of MeHA, the as-prepared microneedle could rapidly extract approximately 1.4 mg of ISF, which was sufficient for the offline detection of metabolites like glucose and cholesterol. Apart from analyzing metabolites, microneedles have also been used to monitor immune cells in the skin. For example, Mandal et al. reported the preparation of a Poly-l-lysine microneedle which was surface-coated with alginate hydrogel containing immunologic adjuvants and antigen, as shown in Figure 6B.[119] Once the microneedle was inserted into the skin, the outmost hydrogel layer swelled. Leukocyte in the skin would infiltrate into the hydrogel and be activated by the embedded adjuvants to recruit T cells into the hydrogel. When the microneedles were removed from the skin, cells could be collected by dissolving the hydrogel layer for immunological analysis. In recent years, polymeric microneedles have been modified with electrochemical sensors or microfluidic chips to achieve real-time in situ monitoring of biomarkers for diagnostic applications.[120–122] For instance, Ciui et al. reported the combination of a wearable wireless bandage sensor with microneedles for in situ melanoma screening.[123] Lee et al. reported the fabrication of thermo-responsive polymeric microneedles combined with glucose sensors for continuous glucose monitoring and on demand drug release.[124] These smart designs endow Figure 7. A) Optical camera image and schematic (bottom) of the wearable sweat-based glucose monitoring patch with the feedback transdermal drug delivery function. Adapted with permission.[124] Copyright 2017, American Association for the Advancement of Science. B) Schematic drawings of the diabetes patch, which is composed of the sweat-control (i, ii), sensing (iii–vii), and therapy (viii–x) components. Adapted with permission.[125] Copyright 2016, Macmillan Publishers Limited. These pioneering works pave the way for the development of closed-loop microneedle-based monitoring and therapeutic delivery systems which consist of sensors and chips. Adv. Therap. 2020, 1900140 1900140 (11 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com the microneedles with the novel characteristic of diagnostic guided therapeutic drug delivery, which would give rise to the revolutionary change in the field of point-of-care medicine. 6. Conclusions and Future Perspectives Currently, great progress has been in the fields of transdermal drug delivery and diagnosis by polymeric microneedles. Novel substrate polymer materials and fabrication techniques are emerging in an endless stream. Polymeric microneedles can not only be administered on demand and release drugs in response to stimulation, but also can be customized individually to improve the patients’ quality of life and achieve better therapeutic effects. With the improvement of people’s living standard and the rapid development of microneedles, development of intelligent and portable microneedle system is the general trend of the times. Stimuli-responsive drug delivery microneedle system, diagnostic and therapeutic integrated microneedle system and wearable microneedle system will become the hotspots in the field of microneedle research. Despite remarkable progress has been made in the development of microneedles for transdermal drug delivery, disease diagnosis and monitoring, the biomedical application of microneedles is still in its infancy, and has not yet moved toward large-scale production and practicality. Some cutting-edge technologies could be integrated with microneedles in the near future. First of all, the vast majority of microneedles-based transdermal drug delivery systems are concerned with the on-demand release of drugs, only limited literatures focus on the combination of microneedles with electrochemical sensors or microchips to realize the closed-loop control of drug release,[124,125] as shown in Figure 7. The ideal circumstance of microneedle-based smart wearable theranostic devices should be like this: the body condition can be monitored in real-time, and once an abnormal situation of the body is found, an early warning will be issued to the patient’s device through the wireless communication system in the microneedle and the drug release system is activated. To achieve such goal, it is of vital importance to integrate microneedles with electronic microchip elements. To fully translate microchip-based microneedle into clinical applications, current microneedle fabrication techniques should be improved to achieve large scale production. Besides, it is necessary to adjust the accuracy and sensitivity of the electronic sensor and effector elements inside the microchip by improving programming and wireless communication techniques. In the future, we envisage that these microneedle-based smart wearable theranostic devices are particularly desirable for medical conditions such as chronic diseases treatment, diabetes management, and control of chronic pain, where long-term application and multistage drug delivery are required. Besides, the current microneedle-based transdermal delivery focuses mainly on delivery of drugs, in the future, microneedles could be utilized for the local delivery of cells to realize cell-based therapy. Nowadays, there are only few researches on the development of cell-loaded microneedles for the treatment of myocardial infarction,[126–128] as shown in Figure 8. In the future, we envisage that microneedles would be widely used to delivery stem cells for organ repair and regeneration. It is also possible to use microneedles as depot for the delivery of probiotics to the intestinal tract to regulate the intestinal microecology for the treatment of some metabolic disease. Some critical issues need to be solved Figure 8. A) Schematic showing the overall design used to test the therapeutic benefits of microneedle- cardiac stromal cells on infarcted heart. Adapted with permission.[128] Copyright 2018, American Association for the Advancement of Science. B) Schematic drawings of transdermal melanocyte delivery using microneedles. Adapted with permission.[127] Copyright 2018, British Association of Dermatologists. These pioneering works pave the way for the future development of cell-integrated microneedles for organ repair and regeneration. Adv. Therap. 2020, 1900140 1900140 (12 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com Figure 9. A) Schematic illustration of microneedle-based transdermal cancer immunotherapy. Adapted with permission.[129] Copyright 2017, American Association for the Advancement of Science. B) Schematic of the MN patch-assisted delivery of a PD1 for the skin cancer treatment. Adapted with permission.[130] Copyright 2016, American Chemical Society. These pioneering works pave the way for the future development of microneedle-based cancer immunotherapy. before realizing such goal, such as how to maintain the cell viability in the microneedle and how to realize uniform distribution of cells within the microneedle. Last but not least, note that immunotherapy in recent years have sparkled increasing interest due to the high treatment efficiency and have been widely utilized in many cutting-edge biomedical fields. Currently, there are already some reports on the application of microneedles to deliver checkpoint inhibitors for tumor treatment,[127,129–131] as shown in Figure 9. In the near future, we envisage that microneedles could be utilized to delivery not only immune inhibitors to treat tumors, but also cytokine and immune cells for on-demand regulation of the microenvironment of the skin and tumor. Considering current advances in the microneedles, it is quite possible to achieve this goal in the near future. With the joint efforts of multi-discipline, it is believed that microneedle-based immunotherapy will sooner or later be utilized for clinical practice. In summary, despite the remarkable achievements that have been made in the microneedle field, development of the next generation’s microneedle-based multifunctional smart biomaterials is still urgently needed for future biomedical applications. It is believed that with the development of science and technology, microneedles will eventually move toward large-scale production and practicality, bringing convenience to people’s lives. We hope that this review would appeal to a broad audience and promote the development of microneedle-based technique for biomedical applications. Acknowledgements This work was financially supported by the Southwest Hospital Key Program (SWH2016ZDCX2014). M.X. thanks the Discovery grant of Natural Science and Engineering Research of Canada and Canada Foundation for Innovation. Conflict of Interest The authors declare no conflict of interest. Adv. Therap. 2020, 1900140 Keywords diagnosis, drug delivery, microneedle fabrication, polymeric microneedles, transdermal delivery Received: July 16, 2019 Revised: October 2, 2019 Published online: [1] D. Chouhan, N. Dey, N. Bhardwaj, B. B. Mandal, Biomaterials 2019, 216, 119267. [2] M. R. Prausnitz, S. Mitragotri, R. Langer, Nat. Rev. Drug Discovery 2004, 3, 115. [3] C. Pegoraro, S. MacNeil, G. Battaglia, Nanoscale 2012, 4, 1881. [4] S. Babity, M. Roohnikan, D. Brambilla, Small 2018, 14, e1803186. [5] M. Amjadi, S. Sheykhansari, B. J. Nelson, M. Sitti, Adv. Mater. 2018, 30, 1704530. [6] E. Larrañeta, M. T. Mccrudden, A. J. Courtenay, R. F. Donnelly, Pharm. Res. 2016, 33, 1055. [7] M. R. Prausnitz, R. Langer, Nat. Biotechnol. 2008, 26, 1261. [8] G. Carneiro, M. G. Aguiar, A. P. Fernandes, L. A. Ferreira, Expert Opin. Drug Delivery 2012, 9, 1083. [9] Y. Ye, K. Haripriya, A. K. Banga, Pharmaceutics 2011, 3, 474. [10] M. R. Prausnitz, V. G. Bose, R. Langer, J. C. Weaver, Proc. Natl. Acad. Sci. U. S. A. 1993, 90, 10504. [11] I. Lavon, J. Kost, Drug Discovery Today 2004, 9, 670. [12] S. Singh, J. Singh, Med. Res. Rev. 2010, 13, 569. [13] J. W. Lee, P. Gadiraju, J. H. Park, M. G. Allen, M. R. Prausnitz, J. Controlled Release 2011, 154, 58. [14] B. M. Medi, J. Singh, Int. J. Pharm. 2006, 308, 61. [15] J. Richter-Johnson, P. Kumar, Y. E. Choonara, L. C. du Toit, V. Pillay, Expert Rev. Pharmacoeconomics Outcomes Res. 2018, 18, 359. [16] K. S. Paudel, M. Milewski, C. L. Swadley, N. K. Brogden, P. Ghosh, A. L. Stinchcomb, Ther. Delivery 2010, 1, 109. [17] Y. Hao, W. Li, X. L. Zhou, F. Yang, Z. Y. Qian, J. Biomed. Nanotechnol. 2017, 13, 1581. [18] T. M. Blicharz, P. Gong, B. M. Bunner, L. L. Chu, K. M. Leonard, J. A. Wakefield, R. E. Williams, M. Dadgar, C. A. Tagliabue, R. El Khaja, S. L. Marlin, R. Haghgooie, S. P. Davis, D. E. Chickering, H. Bernstein, Nat. Biomed. Eng. 2018, 2, 151. 1900140 (13 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com [19] X. Jin, D. D. Zhu, B. Z. Chen, M. Ashfaq, X. D. Guo, Adv. Drug Delivery Rev. 2018, 127, 119. [20] M. R. Prausnitz, Annu. Rev. Chem. Biomol. Eng. 2017, 8, 177. [21] S. P. Davis, B. J. Landis, Z. H. Adams, M. G. Allen, M. R. Prausnitz, J. Biomech. 2004, 37, 1155. [22] E. M. Cahill, E. D. O’Cearbhaill, Bioconjugate Chem. 2015, 26, 1289. [23] M. S. Gerstel, V. A. Place (Alza Corporation), US 3964482, 1976. [24] S. Henry, D. V. McAllister, M. G. Allen, M. R. Prausnitz, J. Pharm. Sci. 1998, 87, 922. [25] K. van der Maaden, W. Jiskoot, J. Bouwstra, J. Controlled Release 2012, 161, 645. [26] M. H. Ling, M. C. Chen, Acta Biomater. 2013, 9, 8952. [27] M. C. Chen, Z. W. Lin, M. H. Ling, ACS Nano 2015, 10, 5b05043. [28] M. C. Chen, M. H. Ling, S. J. Kusuma, Acta Biomater. 2015, 24, 106. [29] S. Yang, W. Fei, J. Liu, G. Fan, W. Welsh, Z. Hua, T. Jin, Adv. Funct. Mater. 2015, 25, 4633. [30] E. Larrañeta, R. E. M. Lutton, A. D. Woolfson, R. F. Donnelly, Mater. Sci. Eng. R 2016, 104, 1. [31] M. Wang, L. Z. Hu, C. J. Xu, Lab Chip 2017, 17, 1373. [32] O. Howells, N. Rajendran, S. Mcintyre, S. Amini-Asl, P. Henri, Y. F. Liu, O. Guy, A. E. G. Cass, M. C. Morris, S. Sharma, ChemBioChem 2019, 17, 20. [33] T. M. Tuan-Mazlelaa, M. T. C. Mccrudden, B. M. Torrisi, M. A. Emma, M. J. Garland, T. R. R. Singh, R. F. Donnelly, Eur. J. Pharm. Sci. 2013, 50, 623. [34] J. Chen, Y. Qiu, S. Zhang, Y. Gao, Drug Dev. Ind. Pharm. 2016, 42, 890. [35] A. P. Raphael, M. L. Crichton, R. J. Falconer, S. Meliga, X. Chen, G. J. Fernando, H. Huang, M. A. Kendall, J. Controlled Release 2016, 225, 40. [36] H. L. Quinn, B. Louise, C. M. Hughes, R. F. Donnelly, J. Pharm. Sci. 2015, 104, 3490. [37] S. Liu, D. Wu, Y. Quan, F. Kamiyama, K. Kusamori, H. Katsumi, T. Sakane, A. Yamamoto, Mol. Pharmaceutics 2015, 13, 272. [38] J. Mönkäre, N. M. Reza, K. Baccouche, S. Romeijn, W. Jiskoot, J. A. Bouwstra, J. Controlled Release 2015, 218, 53. [39] J. Y. Kim, M. R. Han, Y. H. Kim, S. W. Shin, S. Y. Nam, J. H. Park, Eur. J. Pharm. Biopharm. 2016, 105, 148. [40] M. C. Chen, M. H. Ling, K. W. Wang, Z. W. Lin, B. H. Lai, D. H. Chen, Biomacromolecules 2015, 16, 1598. [41] S. Aoyagi, H. Izumi, Y. Isono, M. Fukuda, H. Ogawa, Sens. Actuators A 2007, 139, 293. [42] R. Vecchione, S. Coppola, E. Esposito, C. Casale, V. Vespini, S. Grilli, P. Ferraro, P. A. Netti, Adv. Funct. Mater. 2014, 24, 3515. [43] M. Han, D. H. Hyun, H. H. Park, S. S. Lee, C. H. Kim, C. Kim, J. Micromech. Microeng. 2007, 17, 1184. [44] D. V. Mcallister, M. Ping, Wang, S. P. D, P. Jung-Hwan, P. J. Canatella, M. G. Allen, M. R. Prausnitz, Proc. Natl. Acad. Sci. U. S. A. 2003, 100, 13755. [45] K. T. Tu, C. K. Chung, J. Micromech. Microeng. 2016, 26, 065015. [46] K. J. Cha, T. Kim, S. Jea Park, D. S. Kim, J. Micromech. Microeng. 2014, 24, 115015. [47] M. Kim, B. Jung, J. H. Park, Biomaterials 2012, 33, 668. [48] C. Wang, Y. Ye, G. Hochu, H. Sadeghifa, Z. Gu, Nano Lett. 2016, 16, 2334. [49] L. Wangtan, J. Supaseth, M. Wijuk, C. Muthita, P. Alongkorn, P. Tanapat, S. Werayut, J. Mech. Behav. Biomed. Mater. 2015, 50, 77. [50] S. O. Choi, Y. C. Kim, J. H. Park, J. Hutcheson, H. S. Gill, Y. K. Yoon, M. R. Prausnitz, M. G. Allen, Biomed. Microdevices 2010, 12, 263. [51] R. F. Donnelly, T. R. Singh, M. J. Garland, K. Migalska, R. Majithiya, C. M. McCrudden, P. L. Kole, T. M. Mahmood, H. O. McCarthy, A. D. Woolfson, Adv. Funct. Mater. 2012, 22, 4879. [52] Y. Qiu, G. Qin, S. Zhang, Y. Wu, B. Xu, Y. Gao, Int. J. Pharm. 2012, 437, 51. Adv. Therap. 2020, 1900140 [53] R. F. Donnelly, T. R. Singh, A. Z. Alkilani, M. T. McCrudden, S. O’Neill, C. O’Mahony, K. Armstrong, N. McLoone, P. Kole, A. D. Woolfson, Int. J. Pharm. 2013, 451, 76. [54] R. F. Donnelly, T. R. Singh, M. J. Garland, K. Migalska, R. Majithiya, C. M. Mccrudden, P. L. Kole, T. M. Mahmood, H. O. Mccarthy, A. D. Woolfson, Adv. Funct. Mater. 2012, 22, 4879. [55] K. Y. Lee, J. A. Rowley, P. Eiselt, E. M. Moy, D. J. Mooney, Macromolecules 2000, 33, 4291. [56] S. Y. Yang, E. D. O’Cearbhaill, G. C. Sisk, K. M. Park, W. K. Cho, M. Villiger, B. E. Bouma, B. Pomahac, J. M. Karp, Nat. Commun. 2014, 4, 1702. [57] R. F. Donnelly, M. T. Mccrudden, A. A. Zaid, E. Larrañeta, E. Mcalister, A. J. Courtenay, M. C. Kearney, T. R. Singh, H. O. Mccarthy, V. L. Kett, PLoS One 2014, 9, e111547. [58] A. V. Romanyuk, V. N. Zvezdin, P. Samant, M. I. Grenader, M. Zemlyanova, M. R. Prausnitz, Anal. Chem. 2014, 86, 10520. [59] J. G. Hardy, E. Larraneta, R. F. Donnelly, N. Mcgoldrick, K. Migalska, M. T. Mccrudden, N. J. Irwin, L. Donnelly, C. P. Mccoy, Mol. Pharmaceutics 2016, 13, 907. [60] E. Eltayib, A. J. Brady, E. Caffarelsalvador, P. Gonzalezvazquez, A. Z. Alkilani, H. O. Mccarthy, J. C. Mcelnay, R. F. Donnelly, Eur. J. Pharm. Biopharm. 2016, 102, 123. [61] K. Lee, H. B. Song, W. Cho, J. H. Kim, J. H. Kim, W. Ryu, Acta Biomater. 2018, 80, 48. [62] M. Dangol, H. Yang, G. L. Cheng, S. F. Lahiji, S. Kim, Y. Ma, H. Jung, J. Controlled Release 2016, 223, 118. [63] K. Lee, J. D. Kim, C. Y. Lee, S. Her, H. Jung, Biomaterials 2011, 32, 7705. [64] L. Y. Chu, M. R. Prausnitz, J. Controlled Release 2011, 149, 242. [65] Y. Cao, Y. Tao, Y. Zhou, S. Gui, J. Drug Delivery Sci. Technol. 2016, 35, 1. [66] E. Caffarel-Salvador, R. F. Donnelly, Curr. Pharm. Des. 2016, 22, 1105. [67] S. Duarah, M. Sharma, J. Wen, Eur. J. Pharm. Biopharm. 2019, 136, 48. [68] C. J. Ke, Y. J. Lin, Y. C. Hu, W. L. Chiang, K. J. Chen, W. C. Yang, H. L. Liu, C. C. Fu, H. W. Sung, Biomaterials 2012, 33, 5156. [69] J. Chen, Y. Qiu, S. Zhang, G. Yang, Y. Gao, Drug Dev. Ind. Pharm. 2015, 41, 415. [70] A. M. Rodgers, A. S. Cordeiro, A. Kissenpfennig, R. F. Donnelly, Expert Opin. Drug Delivery 2018, 15, 851. [71] R. L. Creighton, K. A. Woodrow, Adv. Healthcare Mater. 2019, 8, e1801180. [72] D. H. Keum, H. S. Jung, T. Wang, M. H. Shin, Y. E. Kim, K. H. Kim, G. O. Ahn, S. K. Hahn, Adv. Healthcare Mater. 2015, 4, 1152. [73] M. Han, D. K. Kim, S. H. Kang, H. R. Yoon, B. Y. Kim, S. S. Lee, K. D. Kim, H. G. Lee, Sens. Actuators B 2009, 137, 274. [74] S. P. Sullivan, N. Murthy, M. R. Prausnitz, Adv. Mater. 2010, 20, 933. [75] J. D. Kim, M. Kim, H. Yang, K. Lee, H. Jung, J. Controlled Release 2013, 170, 430. [76] K. Lee, H. C. Lee, D. S. Lee, H. Jung, Adv. Mater. 2010, 22, 483. [77] A. R. Johnson, C. L. Caudill, J. R. Tumbleston, C. J. Bloomquist, K. A. Moga, A. Ermoshkin, D. Shirvanyants, S. J. Mecham, J. C. Luft, J. M. Desimone, PLoS One 2016, 11, e0162518. [78] K. Lee, H. Jung, Biomaterials 2012, 33, 7309. [79] Z. Chen, L. Ren, J. Li, L. Yao, Y. Chen, B. Liu, Acta Biomater. 2018, 65, 283. [80] R. D. Pedde, B. Mirani, A. Navaei, T. Styan, S. Wong, M. Mehrali, A. Thakur, N. K. Mohtaram, A. Bayati, A. Dolatshahi-Pirouz, M. Nikkhah, S. M. Willerth, M. Akbari, Adv. Mater. 2017, 29, 1606061. [81] S. H. Lim, J. Y. Ng, L. Kang, Biofabrication 2017, 9, 015010. [82] Afsana, J. V, H. Nafis, J. Keerti, Curr. Pharm. Des. 2018, 24, 5062. [83] C. Y. Liaw, M. Guvendiren, Biofabrication 2017, 9, 024102. [84] J. Giannatsis, V. Dedoussis, Int. J. Adv. Manuf. Technol. 2009, 40, 116. 1900140 (14 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.advancedsciencenews.com www.advtherap.com [85] S. N. Economidou, D. A. Lamprou, D. Douroumis, Int. J. Pharm. 2018, 544, 415. [86] S. M. Barinov, I. V. Vakhrushev, V. S. Komlev, A. V. Mironov, V. K. Popov, A. Y. Teterina, A. Y. Fedotov, K. N. Yarygin, Inorg. Mater.: Appl. Res. 2015, 6, 316. [87] E. A. Allen, C. O’Mahony, M. Cronin, T. O’Mahony, A. C. Moore, A. M. Crean, Int. J. Pharm. 2016, 500, 1. [88] S. Ross, N. Scoutaris, D. Lamprou, D. Mallinson, D. Douroumis, Drug Delivery Transl. Res. 2015, 5, 451. [89] M. Layani, X. Wang, S. Magdassi, Adv. Mater. 2018, 30, e1706344. [90] C. P. P. Pere, S. N. Economidou, G. Lall, C. Ziraud, J. S. Boateng, B. D. Alexander, D. A. Lamprou, D. Douroumis, Int. J. Pharm. 2018, 544, 425. [91] I. Xenikakis, M. Tzimtzimis, K. Tsongas, D. Andreadis, E. Demiri, D. Tzetzis, D. G. Fatouros, Eur. J. Pharm. Sci. 2019, 137, 104976. [92] S. N. Economidou, C. P. P. Pere, A. Reid, M. J. Uddin, J. F. C. Windmill, D. A. Lamprou, D. Douroumis, Mater. Sci. Eng. C 2019, 102, 743. [93] Z. Faraji Rad, R. E. Nordon, C. J. Anthony, L. Bilston, P. D. Prewett, J. Y. Arns, C. H. Arns, L. Zhang, G. J. Davies, Microsyst. Nanoeng. 2017, 3, 17034. [94] M. A. Luzuriaga, D. R. Berry, J. C. Reagan, R. A. Smaldone, J. J. Gassensmith, Lab Chip 2018, 18, 1223. [95] A. Goyanes, J. Wang, A. Buanz, R. Martínez-Pacheco, R. Telford, S. Gaisford, A. W. Basit, Mol. Pharmaceutics 2015, 12, 4077. [96] G. Jonathan, A. Karim, Int. J. Pharm. 2016, 499, 376. [97] J. W. Lee, J. H. Park, M. R. Prausnitz, Biomaterials 2008, 29, 2113. [98] J. H. Park, M. G. Allen, M. R. Prausnitz, J. Controlled Release 2005, 104, 51. [99] M. C. Chen, M. H. Ling, K. Y. Lai, E. Pramudityo, Biomacromolecules 2012, 13, 4022. [100] Z. Z. Zhu, H. F. Luo, W. D. Lu, H. S. Luan, Y. B. Wu, J. Luo, Y. J. Wang, J. X. Pi, C. Y. Lim, H. Wang, Pharm. Res. 2014, 31, 3348. [101] D. D. Zhu, Q. L. Wang, X. B. Liu, X. D. Guo, Acta Biomater. 2016, 41, 312. [102] T. A. Sonia, C. P. Sharma, Adv. Polym. Sci. 2011, 243, 23. [103] D. G. Koutsonanos, M. D. P. Martin, V. G. Zarnitsyn, S. P. Sullivan, R. W. Compans, M. R. Prausnitz, I. Skountzou, PLoS One 2009, 4, e4773. [104] S. Al-Zahrani, M. Zaric, C. Mccrudden, C. Scott, A. Kissenpfennig, R. F. Donnelly, Expert Opin. Drug Delivery 2012, 9, 541. [105] M. C. Chen, S. F. Huang, K. Y. Lai, M. H. Ling, Biomaterials 2013, 34, 3077. [106] W. Li, Y. Liu, J. Du, K. Ren, Y. Wang, Nanoscale 2015, 7, 8476. [107] Q. Zhang, C. Shen, N. Zhao, F. J. Xu, Adv. Funct. Mater. 2017, 27, 1606229. [108] J. Yu, C. Qian, Y. Zhang, Z. Cui, Y. Zhu, Q. Shen, F. S. Ligler, J. B. Buse, Z. Gu, Nano Lett. 2017, 17, 733. [109] Y. Ye, J. Yu, C. Wang, N. Y. Nguyen, G. M. Walker, J. B. Buse, Z. Gu, Adv. Mater. 2016, 28, 3223. [110] J. J. Iliff, N. J. Alkayed, K. J. Gloshani, R. J. Traystman, G. A. West, J. Cereb. Blood Flow Metab. 2005, 25, 1376. Adv. Therap. 2020, 1900140 [111] J. Di, S. Yao, Y. Ye, Z. Cui, J. Yu, T. K. Ghosh, Y. Zhu, Z. Gu, ACS Nano 2015, 9, 9407. [112] J. C. Yu, Y. Q. Zhang, Y. Q. Ye, R. DiSanto, W. J. Sun, D. Ranson, F. S. Ligler, J. B. Buse, Z. Gu, Proc. Natl. Acad. Sci. U. S. A. 2015, 112, 8260. [113] E. V. Mukerjee, S. D. Collins, R. R. Isseroff, R. L. Smith, Sens. Actuators A 2015, 114, 267. [114] G. Zheng, F. Patolsky, C. Yi, W. U. Wang, C. M. Lieber, Nat. Biotechnol. 2005, 23, 1294. [115] A. El-Laboudi, N. S. Oliver, A. Cass, D. Johnston, Diabetes Technol. Ther. 2013, 15, 101. [116] L. Ventrelli, S. L. Marsilio, G. Barillaro, Adv. Healthcare Mater. 2016, 4, 2606. [117] K. W. Ng, W. M. Lau, A. C. Williams, Drug Delivery Transl. Res. 2015, 5, 387. [118] H. Chang, M. J. Zheng, X. J. Yu, A. Than, R. Z. Seeni, R. J. Kang, J. Q. Tian, D. P. Khanh, L. B. Liu, P. Chen, C. J. Xu, Adv. Mater. 2017, 29, 1702243. [119] A. Mandal, A. V. Boopathy, L. K. W. Lam, K. D. Moynihan, M. E. Welch, N. R. Bennett, M. E. Turvey, N. Thai, J. H. Van, J. C. Love, P. T. Hammond, D. J. Irvine, Sci. Transl. Med. 2018, 10, eaar2227. [120] G. Valdés-Ramírez, Y. C. Li, J. Kim, W. Jia, A. J. Bandodkar, R. NuñezFlores, P. R. Miller, S. Y. Wu, R. Narayan, J. R. Windmiller, Electrochem. Commun. 2014, 47, 58. [121] P. R. Miller, X. Xiao, I. Brener, D. B. Burckel, R. Narayan, R. Polsky, Adv. Healthcare Mater. 2014, 3, 876. [122] C. Kolluru, R. Gupta, Q. Jiang, M. Williams, H. Gholami Derami, S. Cao, R. K. Noel, S. Singamaneni, M. R. Prausnitz, ACS Sens. 2019, 4, 1569. [123] B. Ciui, A. Martin, R. K. Mishra, B. Brunetti, T. Nakagawa, T. J. Dawkins, M. Lyu, C. Cristea, R. Sandulescu, J. Wang, Adv. Healthcare Mater. 2018, 7, e1701264. [124] H. Lee, T. K. Choi, Y. B. Lee, H. R. Cho, R. Ghaffari, L. Wang, H. J. Choi, T. D. Chung, N. Lu, T. Hyeon, S. H. Choi, D. H. Kim, Nat. Nanotechnol. 2016, 11, 566. [125] H. Lee, C. Y. Song, Y. S. Hong, M. S. Kim, H. R. Cho, T. Kang, K. Shin, S. H. Choi, T. Hyeon, D. H Kim, Sci. Adv. 2017, 3, e1601314. [126] R. P. Gala, R. U. Zaman, M. J. D’Souza, S. M. Zughaier, Vaccines 2018, 6, 60. [127] B. Gualeni, S. A. Coulman, D. Shah, P. F. Eng, H. Ashraf, P. Vescovo, G. J. Blayney, L. D. Piveteau, O. J. Guy, J. C. Birchall, Br. J. Dermatol. 2018, 178, 731. [128] J. N. Tang, J. Q. Wang, K. Huang, Y. Q. Ye, T. Su, L. Qiao, M. T. Hensley, T. G. Caranasos, J. Y. Zhang, Z. Gu, K. Cheng, Sci. Adv. 2018, 4, eaat9365. [129] Y. Ye, C. Wang, X. Zhang, Q. Hu, Y. Zhang, Q. Liu, D. Wen, J. Milligan, A. Bellotti, L. Huang, G. Dotti, Z. Gu, Sci. Immunol. 2017, 2, eaan5692. [130] C. Wang, Y. Ye, G. M. Hochu, H. Sadeghifar, Z. Gu, Nano Lett. 2016, 16, 2334. [131] H. T. T. Duong, Y. Yin, T. Thambi, T. L. Nguyen, V. H. P. Giang, M. S. Lee, J. E. Lee, J. Kim, J. H. Jeong, D. S. Lee, Biomaterials 2018, 185, 13. 1900140 (15 of 15) © 2020 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim